Orthopedie
U komt op de afdeling Orthopedie, wanneer u een aandoening heeft aandoeningen aan uw botten, spieren of pezen. De afdeling Orthopedie van het LUMC behandelt ook patiënten met een uitgebreide medische voorgeschiedenis en biedt topreferente zorg: zorg waarvoor u niet zomaar in ieder ziekenhuis terecht kunt.
De zorg waarin de afdeling is gespecialiseerd:
- Bot- en wekedelentumoren;
- Plexus Chirurgie;
- Prothese infecties;
- Complexe prothesiologie;
- Bovenste extremiteiten;
- Kinderorthopaedie.
Hoofdthema's
 Bot- en wekedelentumoren
Bot- en wekedelentumoren
De afdeling Orthopaedie van het LUMC is één van de 4 centra in Nederland waar u terecht kunt voor een behandeling van goedaardige en kwaadaardige tumoren van bot en de wekedelen. Omdat deze typen tumoren zeer zeldzame vormen van kanker zijn, is de specialistische zorg hiervoor geconcentreerd in slechts een aantal ziekenhuizen in Nederland, waarvan het LUMC er één is. De afdeling Orthopedie behandelt dan ook patiënten uit het hele land. Zij worden naar het LUMC doorverwezen door artsen uit andere ziekenhuizen. De orthopedisch chirurgen in het LUMC maken gebruik van de nieuwste operatieve technieken en zijn toonaangevend op verschillende gebieden binnen de oncologie. Onder andere op het gebied van computer-genavigeerde ingrepen.
… Bot- en wekedelentumoren
Bot- en wekedelentumoren
De afdeling Orthopaedie van het LUMC is één van de 4 centra in Nederland waar u terecht kunt voor een behandeling van goedaardige en kwaadaardige tumoren van bot en de wekedelen. Omdat deze typen tumoren zeer zeldzame vormen van kanker zijn, is de specialistische zorg hiervoor geconcentreerd in slechts een aantal ziekenhuizen in Nederland, waarvan het LUMC er één is. De afdeling Orthopedie behandelt dan ook patiënten uit het hele land. Zij worden naar het LUMC doorverwezen door artsen uit andere ziekenhuizen. De orthopedisch chirurgen in het LUMC maken gebruik van de nieuwste operatieve technieken en zijn toonaangevend op verschillende gebieden binnen de oncologie. Onder andere op het gebied van computer-genavigeerde ingrepen.
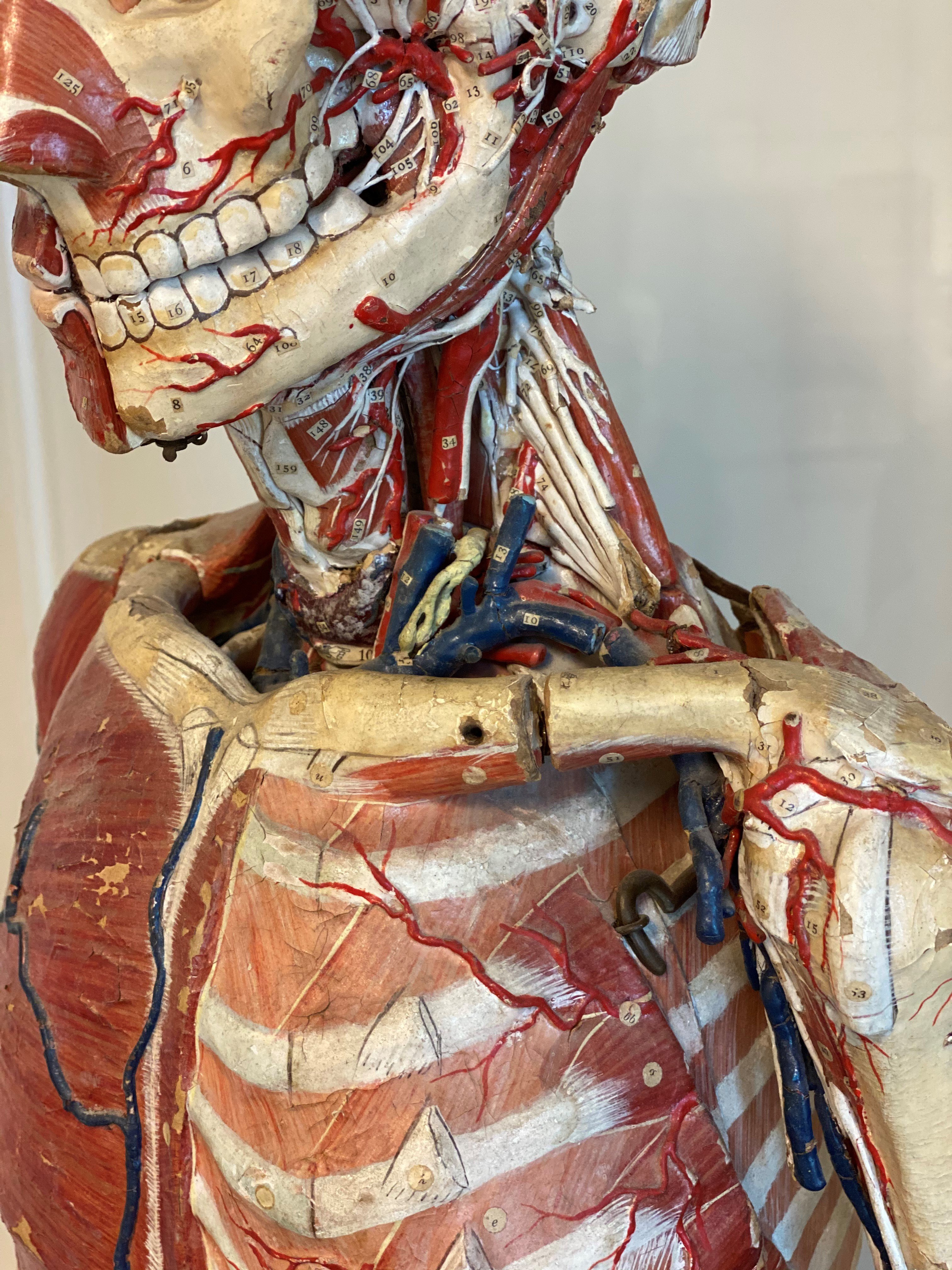 Plexus chirurgie: behandeling van zenuwletsels
Plexus chirurgie: behandeling van zenuwletsels
De behandeling van zenuwletsels is zeldzaam en complex. Er werken daarom meerdere zorgverleners van verschillende disciplines mee aan de benadering. Samen met de bijzondere expertise van de afdeling Orthopedie op dit gebied is dat essentieel voor het slagen van de behandeling. U wordt behandeld door een team bestaande uit een Neurochirurg, Orthopedisch Chirurg, Revalidatiearts en Fysio- of Ergotherapeut. Zij werken in wisselende samenstellingen met elkaar samen.
Het Zenuwcentrum binnen de afdeling Orthopedie is een samenwerkingsverband tussen het LUMC, het Alrijne ziekenhuis en het Nederlands Instituut voor Neurowetenschappen te Amsterdam.
 Prothese infecties
Prothese infecties
Meer dan duizend mensen lopen in Nederland jaarlijks een infectie op aan een gewrichtsprothese. Deze prothese infecties zijn lastig te behandelen. De afdeling Orthopedie van het LUMC brengt alle betrokken medisch specialisten samen, zodat alle kennis over deze prothese infecties gebundeld is. Het team van behandelaars bestaat uit orthopedisch chirurgen, internist-infectiologen en microbiologen. Deze multidisciplinaire behandeling zorgt ervoor dat de beste behandeling wordt gegeven.
Door het combineren van voorlichting, preventie en behandeling willen we de hoeveelheid prothese infecties die voorkomen verminderen en de kans op genezing verbeteren. De afdeling doet ook onderzoek naar nieuwere, patiëntvriendelijker behandelmethodes. Het doel: betere zorg voor patiënten met een prothese.
Thema's
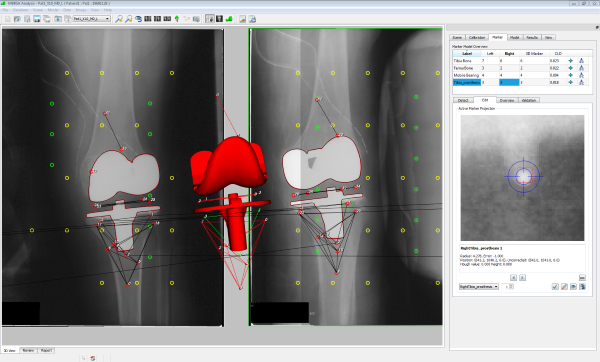
Complexe prothesiologie
Naast gewricht vervangende ingrepen behandelt de afdeling Orthopedie patiënten die een probleem hebben met een eerder geplaatste prothese. Denk hierbij aan:
- Een infectie;
- Het uit de kom schieten;
- Een verkeerde stand van de prothese;
- Loslating;
- Of andere problematiek rondom een gewrichtsprothese.
De orthopedisch chirurgen van het LUMC zijn daarnaast gespecialiseerd in het behandelen en plaatsen van gewrichtsprotheses bij patiënten met aangeboren of verworven afwijkingen aan gewrichten. Er is veel ervaring met het gebruik van innovatieve behandelmogelijkheden zoals computer-genavigeerd opereren en 3D-geprinte hulpmiddelen en implantaten. Doordat de afdeling Orthopedie samenwerkt met veel andere specialisten (bijvoorbeeld infectieartsen, radiologen, microbiologen en fysiotherapeuten) is er veel kennis in huis, voor het stellen van de juiste diagnose een goede behandeling.
…Complexe prothesiologie
Naast gewricht vervangende ingrepen behandelt de afdeling Orthopedie patiënten die een probleem hebben met een eerder geplaatste prothese. Denk hierbij aan:
- Een infectie;
- Het uit de kom schieten;
- Een verkeerde stand van de prothese;
- Loslating;
- Of andere problematiek rondom een gewrichtsprothese.
De orthopedisch chirurgen van het LUMC zijn daarnaast gespecialiseerd in het behandelen en plaatsen van gewrichtsprotheses bij patiënten met aangeboren of verworven afwijkingen aan gewrichten. Er is veel ervaring met het gebruik van innovatieve behandelmogelijkheden zoals computer-genavigeerd opereren en 3D-geprinte hulpmiddelen en implantaten. Doordat de afdeling Orthopedie samenwerkt met veel andere specialisten (bijvoorbeeld infectieartsen, radiologen, microbiologen en fysiotherapeuten) is er veel kennis in huis, voor het stellen van de juiste diagnose een goede behandeling.
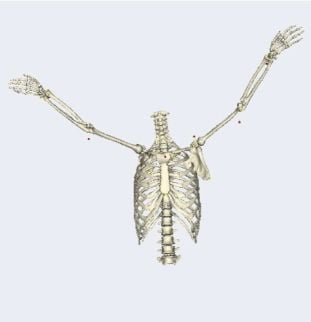
Bovenste extremiteiten
De afdeling Orthopaedie is gespecialiseerd in het behandelen van schouderklachten. De afdeling heeft zich met name toegelegd op:
- Peesletsels van spieren rond het schoudergewricht;
- Coördinatiestoornissen;
- Artrose of reumatische aandoeningen van het schoudergewricht’
- En problemen met het functioneren na een schoudervervangende operatie (schouderprothese).
De behandelingen bestaan uit onder andere oefentherapie, lokale injecties, gewrichtsvervangende operaties en peesherstel- of peesverplaatsingsoperaties.
Kinderorthopedie
De kinderorthopedie houdt zich bezig met afwijkingen van de botten, gewrichten, banden, spieren en pezen van kinderen tot 18 jaar. Hierbij gaat het bijvoorbeeld om:
- Aangeboren ziekten;
- Groei-afwijkingen;
- Botbreuken;
- Infecties (osteomyelitis, artritis);
- Of zeldzame ziektes als tumoren.
Polikliniek en verpleegafdeling
De afdeling Orthopedie van het Leids Universitair Medisch Centrum (LUMC) is onderdeel van de ROGO West en leidt samen met het Haaglanden Medisch Centrum en het Reinier Haga Orthopedisch Centrum dokters op tot orthopedisch chirurg.
Daarnaast levert de afdeling Orthopedie een intensieve bijdrage aan het onderwijs van drie bacheloropleidingen en zes masteropleidingen van de Universiteit Leiden en de TU delft en aan postacademisch onderwijs.
Opleidingen
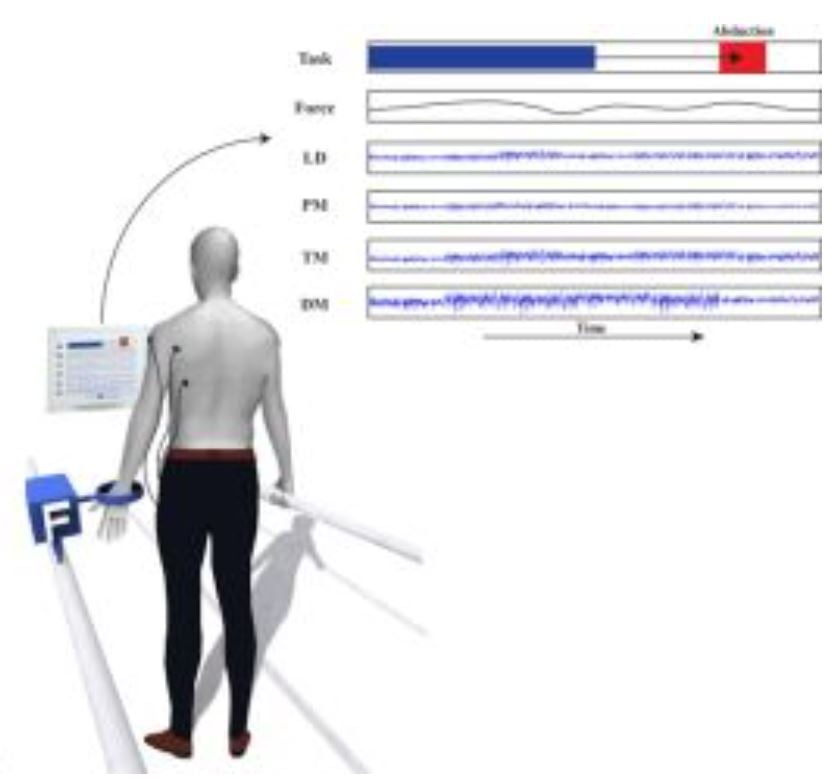
Physical impairments and limitations of mobility have a major impact on the independency and quality of life of many persons and pose a large economic burden to society. In the Netherlands annually about 75.000 patients have a knee or hip arthroplasty, 55.000 sustain a hip, ankle or wrist fracture, more than 25.000 suffering from a stroke and about 3000 patients diagnosed with bone and soft tissue tumors. All with varying clinical outcome after varying interventions surgical as well as conservative. Research is focused on the clinical expertise areas as defined by the 10 LUMC Research Themes. The overarching research theme of "Mobility", encompassing Musculoskeletal (MSK) pathology and Brain and nerve injuries results from the overarching denominator of musculoskeletal and neurosciences. Unsatisfactory outcomes and complications are common in all designated subgroups of patients, leading to significant health care usage and loss of productivity. In order to address these issues, the research program focusses on two research themes: "Prognostic Clinical Modelling" and "Optimising Clinical Outcome".
The research program is built on the extensive experience of the involved clinical networks as well as methodological expertise in the development, evaluation and implementation of complex care and technology.
Research programs
Projecten en publicaties
Meer informatie
Missie
Onze missie is “Grensverleggend Beter Worden”, een dynamisch proces dat continu in beweging is, zeker voor de afdeling Orthopaedie, Revalidatiegeneeskunde en Fysiotherapie. Hierbij is niet alleen het samenwerken op zichzelf, maar verbinden het belangrijkste element. Dit laatste stimuleert niet alleen het beter worden, maar is essentieel voor het Grensverleggend Beter Worden binnen de patiëntenzorg, onderwijs & opleiding en onderzoek.
Werken bij
De afdeling Orthopaedie begeleidt het gehele jaar door wetenschapsstudenten. Interesse in een wetenschapsstage of wil je ervaring opdoen op het gebied van wetenschappelijk onderzoek? Stuur dan een mailtje naar orthopaedie@lumc.nl
Ook zijn er regelmatig onderzoeksvacatures. Op dit moment zijn wij op zoek naar een promovendus/arts-onderzoeker op het gebied van Zorgevaluatie binnen onze afdeling Orthopaedie.
Kijk voor meer informatie over deze en andere vacatures op Werken Bij.
Behandelteam
Medische staf
- Prof.dr. Rob (R.G.H.H.) Nelissen
Orthopaedisch Chirurg - Afdelingshoofd - Plaatsvervangend opleider
Perifeer zenuwletsel - Complexe gewrichtsreconstructie (incl. infecties) - Bovenste Extremiteit - Prof. dr. Bart (B.C.H.) van der Wal
Orthopaedisch Chirurg
Heup en knierevisies - Prof. dr. Michiel (M.A.J.) van de Sande
Orthopaedisch Chirurg
Oncologische Orthopaedie - Kinderorthopaedie - Dr. Enrike (H.M.J.) van der Linden-van der Zwaag
Orthopaedisch Chirurg
Algemene Orthopaedie - Complexe gewrichtsreconstructie (incl. infecties) - Michaël (M.P.A.) Bus
Orthopaedisch chirurg
Oncologische orthopaedie – Infecties – Traumatologie - Drs.Jochem (J.) Nagels
Orthopaedisch Chirurg
Perifeer Zenuwletsel - Complexe gewrichtsreconstructie (incl. infecties) - Bovenste Extremiteit - Opleider - Dr. Robert (R.J.P.) van der Wal
Orthopaedisch Chirurg
Oncologische Orthopaedie - Complexe gewrichtsreconstructie (incl. infecties) - Wervelkolom - Demien Broekhuis
Orthopaedisch Chirurg
Oncologische Orthopaedie - Complexe gewrichtsreconstructie (incl. infecties) - Traumatologie - Dagmar (D.R.J.) Kempink
Orthopaedisch Chirurg
Kinderorthopaedie - Banne Németh
Orthopaedisch chirurg
Perifeer zenuwletsel - Complexe gewrichtsreconstructie (incl. infecties) - Bovenste Extremiteit - Dr. Pieter Bas de Witte
Orthopaedisch Chirurg
Kinderorthopaedie - Gewrichtsreconstructies -Traumatologie - Dr. Jasper (J.G.) Gerbers
Orthopaedisch chirurg, met als specialisatie oncologie, complexe gewrichtsreconstructie (incl. infectie) en traumatologie.
Medische staf
- Prof.dr. Rob (R.G.H.H.) Nelissen
Orthopaedisch Chirurg - Afdelingshoofd - Plaatsvervangend opleider
Perifeer zenuwletsel - Complexe gewrichtsreconstructie (incl. infecties) - Bovenste Extremiteit - Prof. dr. Bart (B.C.H.) van der Wal
Orthopaedisch Chirurg
Heup en knierevisies - Prof. dr. Michiel (M.A.J.) van de Sande
Orthopaedisch Chirurg
Oncologische Orthopaedie - Kinderorthopaedie - Dr. Enrike (H.M.J.) van der Linden-van der Zwaag
Orthopaedisch Chirurg
Algemene Orthopaedie - Complexe gewrichtsreconstructie (incl. infecties) - Michaël (M.P.A.) Bus
Orthopaedisch chirurg
Oncologische orthopaedie – Infecties – Traumatologie - Drs.Jochem (J.) Nagels
Orthopaedisch Chirurg
Perifeer Zenuwletsel - Complexe gewrichtsreconstructie (incl. infecties) - Bovenste Extremiteit - Opleider - Dr. Robert (R.J.P.) van der Wal
Orthopaedisch Chirurg
Oncologische Orthopaedie - Complexe gewrichtsreconstructie (incl. infecties) - Wervelkolom - Demien Broekhuis
Orthopaedisch Chirurg
Oncologische Orthopaedie - Complexe gewrichtsreconstructie (incl. infecties) - Traumatologie - Dagmar (D.R.J.) Kempink
Orthopaedisch Chirurg
Kinderorthopaedie - Banne Németh
Orthopaedisch chirurg
Perifeer zenuwletsel - Complexe gewrichtsreconstructie (incl. infecties) - Bovenste Extremiteit - Dr. Pieter Bas de Witte
Orthopaedisch Chirurg
Kinderorthopaedie - Gewrichtsreconstructies -Traumatologie - Dr. Jasper (J.G.) Gerbers
Orthopaedisch chirurg, met als specialisatie oncologie, complexe gewrichtsreconstructie (incl. infectie) en traumatologie.
Orthopaedisch chirurg in opleiding
- Julie Herfkens
Orthopaedisch Chirurg in Opleiding - Lilian Donders
Orthopaedisch Chirurg in Opleiding - Hamez Gacaferi
Orthopaedisch Chirurg in Opleiding - Kim Spierings
Orthopaedisch Chirurg in Opleiding - Kayou Azizpour
Orthopaedisch Chirurg in Opleiding
Assistent Niet in Opleiding (ANIOS)
- Lotje (L.A.) Hoogervorst
- Merel Roelen
Verpleegkundig Assistent
- Nicolette (N.A.C.) Leijerzapf
Verpleegkundig Specialist - Marloes van Duijvenbode
Verpleegkundig Specialist - Nardy (B.A.C) de Wit-Dubois
Verpleegkundig Specialist in Opleiding
Wetenschappelijke staf
- Prof.dr. Thea (T.P.M.) Vliet Vlieland
Hoogleraar - Prof.dr. Rudolf (R.W.) Poolman
Hoogleraar - Prof.dr. Frans (F.C.T.) van der Helm
Hoogleraar - Prof.dr.ir. Jaap Harlaar
Hoogleraar - Prof.dr. Amir (A.A.) Zadpoor
Hoogleraar - Dr.ir. Bart (B.L.) Kaptein
Assistant professor - Dr. Maaike (M.G.J.) Gademan
Associate professor - Lennard (L.A.) Koster
Onderzoeker - Bart Pijls
Dr. Bart (B.G.C.W.) Pijls
Assistant professor
Onderzoekers
- Ruben Kok
Arts-Onderzoeker - Hilde (H.W.) van Kouswijk
Onderzoeker-in-Opleiding - Lisa van der Water
Arts-onderzoeker - Sjors van de Vusse
Arts-onderzoeker - Claire Scholte
PhD student - Douwe Rijntjes
Arts-onderzoeker - Julia (J.F.) van der Geest
Onderzoeker-in-Opleiding
PostDoc
- Melisa Castañeda Vanegas
Stafsecretariaat
- Annemieke Stolk
Management-assistente - Anika (A.J.) Rabelink-Hoogenstraaten
Datamanager - Eveline Prins
Secretaresse
&width=180&height=180)
&width=180&height=180)
&width=180&height=180)