Neurologie
&width=710&height=710)
Om u de allerbeste zorg te bieden, hebben de medewerkers van de Neurologie van het LUMC zich extra gespecialiseerd in een aantal specifieke neurologische ziekten. Om nog meer kennis op te doen over deze aandoeningen wordt ook wetenschappelijk onderzoek verricht naar deze neurologische ziekten:
- Beroerte (herseninfarct, hersenbloeding, cerebrale amyloid angiopathie);
- Erfelijke aandoeningen van de (kleine) bloedvaten in de hersenen (denk aan HCHWA-D, RVCL-S);
- Hersentumoren (zoals gliomen en uitzaaiingen naar de hersenen);
- Bewegingsstoornissen (de ziekte van Huntington, de ziekte van Parkinson);
- Neuromusculaire aandoeningen (denk hierbij aan myasthenia gravis, Duchenne spierdystrofie);
- Hoofdpijn syndromen (migraine, clusterhoofdpijn);
- Wegrakingen door een stoornis van het autonoom zenuwstelsel;
- Kinderneurologische aandoeningen.
Om u de allerbeste zorg te bieden, hebben de medewerkers van de Neurologie van het LUMC zich extra gespecialiseerd in een aantal specifieke neurologische ziekten. Om nog meer kennis op te doen over deze aandoeningen wordt ook wetenschappelijk onderzoek verricht naar deze neurologische ziekten:
- Beroerte (herseninfarct, hersenbloeding, cerebrale amyloid angiopathie);
- Erfelijke aandoeningen van de (kleine) bloedvaten in de hersenen (denk aan HCHWA-D, RVCL-S);
- Hersentumoren (zoals gliomen en uitzaaiingen naar de hersenen);
- Bewegingsstoornissen (de ziekte van Huntington, de ziekte van Parkinson);
- Neuromusculaire aandoeningen (denk hierbij aan myasthenia gravis, Duchenne spierdystrofie);
- Hoofdpijn syndromen (migraine, clusterhoofdpijn);
- Wegrakingen door een stoornis van het autonoom zenuwstelsel;
- Kinderneurologische aandoeningen.
Kinderen en Neurologie
Kinderen met neurologische aandoeningen worden verpleegd op de kinderafdeling Bos of Strand op J-6. Voor meer informatie over de behandeling van kinderen kijkt u op de website van de afdeling kindergeneeskunde.
Onze kennis
Als experts op het gebied van neurologische aandoeningen zien wij het als onze taak niet alleen de meest recente kennis van zaken te hebben, maar ook om bij te dragen aan uitbreiding van deze kennis en deze kennis te delen met de rest van de wereld.
De afdeling Neurologie doet veel hoogstaand wetenschappelijk onderzoek. Al dan niet in samenwerking met andere afdelingen en instituten. Wij kunnen u daarom vragen mee te werken aan wetenschappelijk onderzoek. Nadat u uitleg heeft gekregen over de inhoud van het onderzoek krijgt u schriftelijke informatie mee die u kunt nalezen. U krijgt ruim de tijd na te denken of u aan het onderzoek mee wilt werken. Al het wetenschappelijk onderzoek vindt pas plaats na instemming door een wetenschapscommissie, een Medische Ethische Toetsingscommissie en de Raad van Bestuur van het LUMC.
…Als experts op het gebied van neurologische aandoeningen zien wij het als onze taak niet alleen de meest recente kennis van zaken te hebben, maar ook om bij te dragen aan uitbreiding van deze kennis en deze kennis te delen met de rest van de wereld.
De afdeling Neurologie doet veel hoogstaand wetenschappelijk onderzoek. Al dan niet in samenwerking met andere afdelingen en instituten. Wij kunnen u daarom vragen mee te werken aan wetenschappelijk onderzoek. Nadat u uitleg heeft gekregen over de inhoud van het onderzoek krijgt u schriftelijke informatie mee die u kunt nalezen. U krijgt ruim de tijd na te denken of u aan het onderzoek mee wilt werken. Al het wetenschappelijk onderzoek vindt pas plaats na instemming door een wetenschapscommissie, een Medische Ethische Toetsingscommissie en de Raad van Bestuur van het LUMC.
Het LUMC is een Universitair Medisch Centrum. Dat betekent dat er niet alleen patiëntenzorg, maar ook onderwijs wordt gegeven. Het is daarom mogelijk dat medewerkers soms een stagiaire bij zich hebben. Indien het voor onderwijsdoeleinden nodig is om deze personen bij uw behandeling te betrekken, zult u hiervan op de hoogte gesteld worden. Ook kunt u gevraagd worden om deel te nemen aan onderwijsleermomenten.
De afdeling neurologie draagt bij aan de opleidingen geneeskunde, biomedische wetenschappen en klinische technologie. Daarnaast worden artsen opgeleid tot (kinder)neuroloog en wetenschappelijk onderzoeker. Er wordt bijgedragen aan kennisbevordering van collegae in het LUMC, nationaal en internationaal.
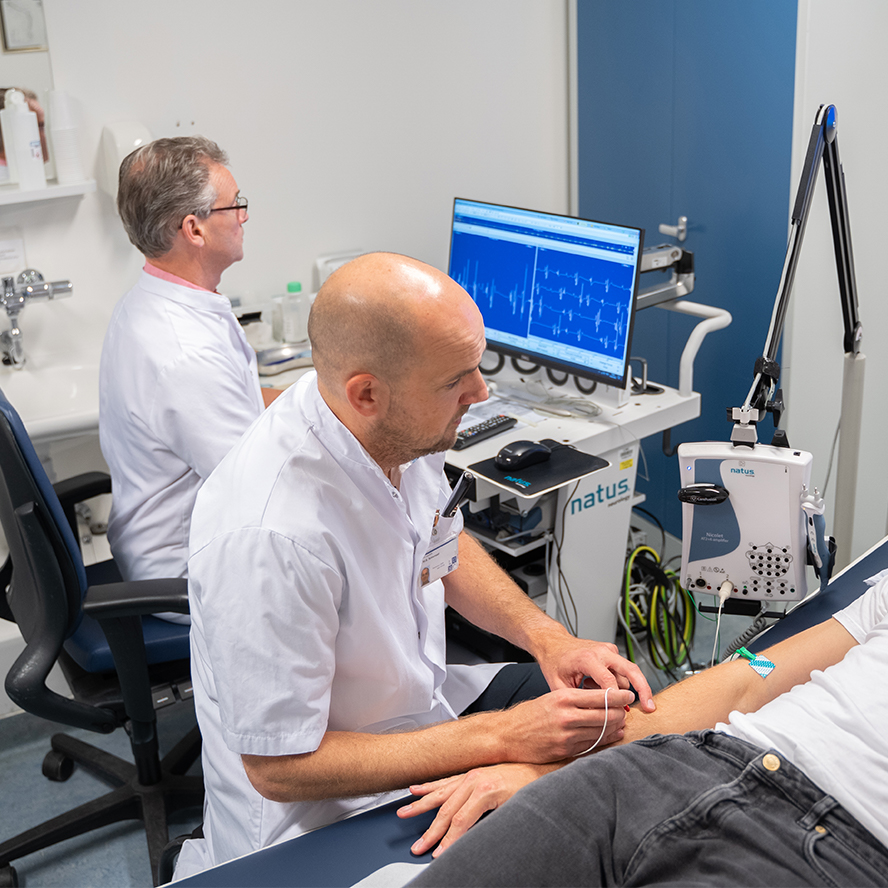
Op de klinische afdeling worden verpleegkundigen en physician assistants opgeleid, op de subafdelingen neuropsychologie worden psychologen opgeleid en op de klinische neurofysiologie worden laboranten opgeleid.
Opleidingen
Neurology is that part of medical science that is concerned with disorders of the central (brain and spine) and peripheral nervous system (nerves, neuromuscular junction, muscles). Our ambition is to perform high quality research that competes at the top international level and has a close relationship with patient care and education within the LUMC.
Research theme
In the LUMC different specialists collaborate around research themes of which there are 10: Academic Pharma, Cancer, Cardiovascular, Cell Tissue & Organ Transplantation, Immunity, Infection, Life course, Medical Genomics, Neuroscience, Prevention and Lifestyle. The department of Neurology participates in many of these themes but its major focus is on the Neuroscience theme.
Neurology is that part of medical science that is concerned with disorders of the central (brain and spine) and peripheral nervous system (nerves, neuromuscular junction, muscles). Our ambition is to perform high quality research that competes at the top international level and has a close relationship with patient care and education within the LUMC.
Research theme
In the LUMC different specialists collaborate around research themes of which there are 10: Academic Pharma, Cancer, Cardiovascular, Cell Tissue & Organ Transplantation, Immunity, Infection, Life course, Medical Genomics, Neuroscience, Prevention and Lifestyle. The department of Neurology participates in many of these themes but its major focus is on the Neuroscience theme.
With the development of the Neuroscience theme a scientific community is being created for all researchers working on neuroscience in the LUMC to enhance collaboration, promote research activities, and to cultivate a new generation of young scientists. The most auspicious and successful research lines have now been divided into 12 subthemes.
Research subthemes or research programmes
Paroxysmal Cerebral Disorders (PaCD), Neurovascular Disorders, Movement Disorders, Muscle & Synapse Disorders and Neuro-Oncology are 5 of the subthemes that are the main focus of our department and the research programmes connected to them have the same entitlement.
Participation in research
Students
We have multiple opportunities for students to conduct research at our department, especially for those in the discipline of Medicine, Biomedical Sciences, and Clinical Technology. If you are interested in any of the topics related to the research subthemes feel free to ask us for a scientific internship. Contact our research secretariat, fill in the inventory form and send along a curriculum vitae. The forms will be forwarded to the principal investigators specialized on the topic of your preference and we will try to reply within 3 weeks.
…Students
We have multiple opportunities for students to conduct research at our department, especially for those in the discipline of Medicine, Biomedical Sciences, and Clinical Technology. If you are interested in any of the topics related to the research subthemes feel free to ask us for a scientific internship. Contact our research secretariat, fill in the inventory form and send along a curriculum vitae. The forms will be forwarded to the principal investigators specialized on the topic of your preference and we will try to reply within 3 weeks.
We also have opportunities for PhD trajectories on the topics mentioned before. Ask us for more information if you are interested.
National and international collaborators
The Department of Neurology has an extensive operational and collaborative network. A number of collaborations have been formalized by appointment of researchers that have their main activities in other institutions as affiliated professor at our Department. Do not hesitate to contact us if you would like to investigate opportunities for collaboration.
Pharma
The department of Neurology not only carries out numerous preclinical and clinical studies in all phases together with our basic science partners, but is also involved in advisory boards when therapies are being developed. To help you on your way to engage to one of our principal investigators feel free to contact our secretariat.
Contact: Research Administration
Location: K-5-Q
Telephone: +31-(0)715262895
Availability: Monday to Friday from 8.30-17.00.
E-mail: stafsecretariaatneurologie@lumc.nl or c.j.m.van_brunschot@lumc.nl
Research programs
Research groups
Onderzoek naar de ziekte van Duchenne/Becker
In het LUMC wordt vanuit verschillende disciplines onderzoek gedaan naar Duchenne en/of Becker spierdystrofie. Dit betreft zowel onderzoek in het laboratorium als onderzoeken bij patiënten. Naast onderzoek gericht op behandeling van de spierdystrofieën wordt er in het LUMC ook onderzoek gedaan naar bijvoorbeeld het voorkomen en de kenmerken van spierdystrofieën.
Onderstaande pagina is bedoeld voor mensen met de ziekte van Duchenne/Becker en hun familie. Hier vindt u informatie over de onderzoeken die in het LUMC plaatsvinden naar deze ziektes.
Contactgegevens
Polikliniek secretariaat Volwassenen
Locatie: J-3-Q
Telefoon: +31 (0)71 526 21 11 (toets 2)
Bereikbaar: maandag t/m vrijdag van 8.15 uur -11.30 uur
E-mail: polineurologie@lumc.nl
Polikliniek secretariaat Kinderneurologie
Locatie: J-3-R
Telefoon: +31 (0)71 526 21 11 (toets 1)
Bereikbaar: maandag t/m vrijdag van 8.15 uur -11.30 uur
Email: polikinderneurologie@lumc.nl
Polikliniek secretariaat Volwassenen
Locatie: J-3-Q
Telefoon: +31 (0)71 526 21 11 (toets 2)
Bereikbaar: maandag t/m vrijdag van 8.15 uur -11.30 uur
E-mail: polineurologie@lumc.nl
Polikliniek secretariaat Kinderneurologie
Locatie: J-3-R
Telefoon: +31 (0)71 526 21 11 (toets 1)
Bereikbaar: maandag t/m vrijdag van 8.15 uur -11.30 uur
Email: polikinderneurologie@lumc.nl
Secretariaat Klinische Neurofysiologie
Locatie: J-3-R
Telefoon: +31 (0)71 526 21 11 (toets 3)
Bereikbaar: maandag t/m vrijdag van 8.15 uur -11.30 uur
Secretariaat Neuropsychologie
Locatie: J-3-R
Telefoon: +31 (0)71 526 21 11 (toets 4)
Bereikbaar: maandag t/m vrijdag van 8.15 uur -11.30 uur
Kliniek secretariaat (verpleegafdeling en Neurocare)
Locatie: J-10-P (verpleegafdeling), J-11-P (Neurocare)
Telefoon: +31 (0)71 526 53 48
Bereikbaar: maandag t/m vrijdag van 7.30 uur -17.00 uur
Email: neurologie@lumc.nl
Balie verpleging (verpleegafdeling en Neurocare)
Locatie: J-10-P (verpleegafdeling), J-11-Q (Neurocare)
Telefoon:+31 (0)71 526 26 47 (verpleegafdeling)/+31 (0)71 526 21 21 (Neurocare)
Bereikbaar: dagelijks
Stafsecretariaat neurologie
Locatie: K-5-Q
Telefoon: +31 (0)71 526 21 97
Bereikbaar: maandag t/m vrijdag van 8.30 uur-17.00 uur
E-mail: stafsecretariaatneurolgie@lumc.nl
Onderwijs secretariaat
Locatie: K-5-Q
Telefoon: +31 (0)71 526 28 95 of +31 (0)71 526 21 34
Bereikbaar: maandag t/m vrijdag van 8.30 uur -17.00 uur
E-mail: stafsecretariaatneurologie@lumc.nl
Research secretariaat
Locatie: K-5-Q
Telefoon: +31 (0)71 526 28 95
Bereikbaar: maandag t/m vrijdag van 8.30 uur-17.00 uur
E-mail: stafsecretariaatneurolgie@lumc.nl
Spoedoverleg (voor verwijzers)
Spoedoverleg poliklinische verwijzing (< 1 week):
Telefoon: +31 (0)71 526 91 11 en pieper 99235
Bereikbaar: maandag t/m vrijdag 08.45-17.00
Spoedoverleg SEH verwijzing (zelfde dag):
Telefoon: +31 (0)71-526 91 11 en pieper 99234 (08.30 uur-17.00 uur, maandag t/m vrijdag), pieper 99570 tijdens diensturen (17.00-08.30 uur en weekend)
Bereikbaar: dagelijks
Spoedoverleg TIA analyse verwijzing
Telefoon: +31 (0)71-526 91 11 en pieper 98048
Bereikbaar: maandag t/m vrijdag van 08.30-17.00 uur en op overige tijdstippen via pieper 99570
&width=180&height=180)
&width=180&height=180)
&width=180&height=180)