Klinische Genetica
&width=710&height=710)
Patiëntenzorg is de kern van de bezigheden van de afdeling Klinische Genetica. Wij zien patiënten met vraagstellingen over erfelijkheid op de polikliniek, en verrichten genetische diagnostiek in ons laboratorium.
Voor patiënten
Een klinisch geneticus of andere klinisch-genetische zorgprofessional zoekt voor u uit of een aandoening erfelijk is. Er wordt onderzocht of er een verhoogde kans is voor uzelf of uw kinderen en zonodig wordt er DNA-diagnostiek aangevraagd. Zij bespreken de uitkomst van het onderzoek en de eventuele gevolgen voor u en uw familieleden.
In specifieke situaties bieden wij tevens psychologische begeleiding aan bij persoonlijke keuzes die u moet maken. Het kan zijn dat uw familieleden belang hebben bij de uitkomst van het erfelijkheidsonderzoek. In dat geval vragen wij u uw familie te informeren. Eventueel kunnen wij daarbij behulpzaam zijn.
Voor meer informatie over de polikliniek Klinische Genetica en de diverse spreekuren die wij doen kunt u hier klikken.
Voor aanvragers
De sectie Genoomdiagnostiek (GD) is verantwoordelijk voor de uitvoering en interpretatie van diagnostiek op het gebied van een groot aantal aandoeningen. Het GD is ISO15189 geaccrediteerd door de Raad voor Accreditatie onder nummer M007. De aanvraagformulieren en meer informatie over onze diagnostische werkzaamheden vindt u hieronder.
Voor meer informatie over het aanvragen van diagnostiek door niet-klinisch genetische zorgprofessionals verwijzen wij graag naar Leidraad aanvragen genetische diagnostiek in de kiembaan doorniet klinisch genetische zorgprofessionals.pdf (vkgn.org) en de pagina Zelf diagnostiek aanvragen | Arts en Genetica .
Meer informatie over nevenbevindingen vindt u op Nevenbevindingen | Arts en Genetica
De afdeling Klinische Genetica levert een actieve bijdrage aan de onderwijstaken van het LUMC op het vakgebied van erfelijkheidadvisering en klinisch genetische laboratorium diagnostiek. Dit bestaat uit onderwijs binnen het curriculum geneeskunde en biomedische wetenschappen (organisatie van blokken en lijnonderwijs, en het aanbieden van stageplaatsen), postacademisch onderwijs aan diverse specialismen en huisartsen.
Opleidingen
Clinical Genetics underlines the research goal of this centre which is: “To elucidate the molecular and clinical etiology of hereditary disease, congenital malformation, multifactorial disorders and hereditary cancer, in order to improve diagnostics, assist counselling, develop treatments and further prevention.”
Research programs
Contactgegevens
Polikliniek Klinische Genetica
Intercollegiaal overleg
Telefoonnummer: 071 526 10 92
Patiëntenzorgsecretariaat
Voor afspraken en vragen kunt u contact opnemen met:
Telefoonnummer: 071 526 80 33
E-mail: genetica@lumc.nl
Sectie Genoomdiagnostiek
Einthovenweg 20, 2333 ZC Leiden
Postbus 9600, 2300 RC Leiden
Gebouw 2, S6-P
Monsterontvangst
Zorgverleners kunnen van maandag t/m vrijdag contact opnemen met:
Telefoon: 071 526 98 00 bereikbaar van 8.30-12.30 en 13.30- 17.00 uur
E-mail: genoomdiagnostiek@lumc.nl
Stafsecretariaat
Telefoon: 071 526 98 10
E-mail: stafsecretariaat.kg@lumc.nl
Kwaliteit en accreditatie
Accreditatie Laboratorium
Het GD bestaat uit verschillende disciplines met een laboratoriumbreed kwaliteitszorgsysteem, gebaseerd op de internationale norm ISO 15189. Het LDGA met registratienummer M007 is sinds oktober 2006 geaccrediteerd door de RvA.
Accreditatie historie Laboratorium
…Accreditatie Laboratorium
Het GD bestaat uit verschillende disciplines met een laboratoriumbreed kwaliteitszorgsysteem, gebaseerd op de internationale norm ISO 15189. Het LDGA met registratienummer M007 is sinds oktober 2006 geaccrediteerd door de RvA.
Accreditatie historie Laboratorium
Moleculaire Genetica is sinds 1998 in het bezit van een RvA accreditatie, op basis van ISO 17025 (inclusief ISO 9001).
Cytogenetica is in 2000 geaccrediteerd door zowel CCKL (Stichting voor de bevordering van de kwaliteit van het laboratoriumonderzoek en voor accreditatie van laboratoria in de gezondheidszorg) als de RvA. Beide laboratoria waren als eerste in hun vakgebied geaccrediteerd. De CCKL erkenning is per 1 januari 2008 vrijwillig opgezegd. De reden van de opzegging was dat CCKL, in tegenstelling tot de RVA, geen internationale erkenning kan en mag afgeven.
Het Hemoglobinopathieën Laboratorium is sinds 2006 geaccrediteerd door de RvA. Zie de lijst van geaccrediteerde verrichtingen van het LDGA.
Kwaliteitsborging in de praktijk binnen het LDGA
De kwaliteitsborging binnen de laboratoria is gericht op het voorkomen van monsterverwisselingen en het produceren van betrouwbare en reproduceerbare resultaten. Alle gebruikte methodes en technieken zijn gevalideerd en beschreven.
In het primaire proces zijn, waar mogelijk, controles ingebouwd om verwisselingen te voorkomen. De beschrijving van het werkproces gecombineerd met een uitvoerige interne opleiding van de medewerkers vormen de belangrijkste pijlers in de diagnostiek.
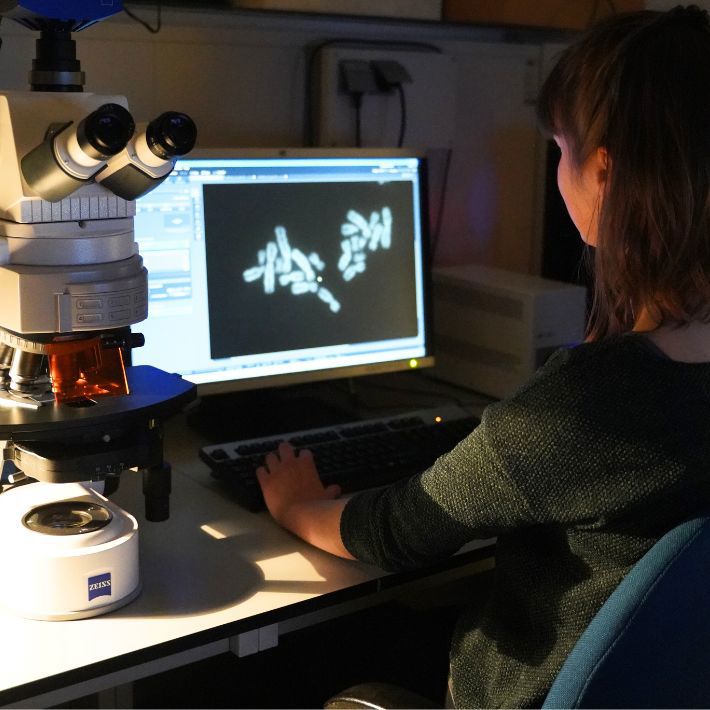
De cytogenetische kwaliteitsborging: is afhankelijk van goede chromosoompreparaten en deskundige analisten, die de mogelijke chromosomale afwijkingen kunnen opsporen en herkennen.
Voor moleculaire analyses worden twee buizen bloed van dezelfde patiënt na binnenkomst gescheiden opgewerkt tot twee duplo DNA monsters, met ieder een eigen monstercode. Elke bevinding voor directe mutatie analyse wordt bevestigd op dit tweede monster, alvorens het resultaat wordt vrijgegeven. Het meenemen van positieve en negatieve controles en een gedocumenteerd intern opleidingstraject waarborgt de reproduceerbaarheid van de resultaten.
Daarnaast participeert het laboratorium in diverse ringonderzoeken in Europees verband en organiseert het laboratorium de ringonderzoeken voor een tweetal frequente erfelijke aandoeningen.
&width=180&height=180)
&width=180&height=180)
&width=180&height=180)