Parasitologie
Leiden Malaria Research Group
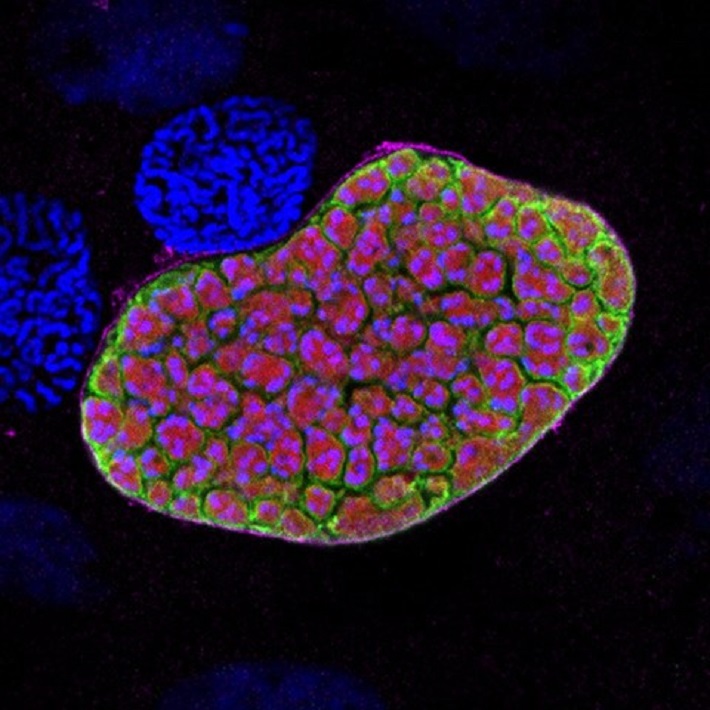
Our studies are aimed at developing interventions against human malaria; both by examining and manipulating the human malaria-parasite Plasmodium falciparum, and by exploiting rodent models of malaria parasites (Plasmodium berghei, P. yoelii). This research, embedded in the research themes ‘Infection’ and ‘Immunity’ of the Department is performed under supervision of Dr. Chris J. Janse and Dr. Blandine Franke-Fayard.
Main research themes
- Development of a malaria vaccine based on genetically attenuated parasites (GAP vaccine)
- Identification and analysis of parasite proteins that are (putative) targets for subunit vaccines
- Identification and analysis of parasite proteins that are (putative) targets for drugs
- Analysis of parasite-host interactions involved in pathology and disease
Main research themes
- Development of a malaria vaccine based on genetically attenuated parasites (GAP vaccine)
- Identification and analysis of parasite proteins that are (putative) targets for subunit vaccines
- Identification and analysis of parasite proteins that are (putative) targets for drugs
- Analysis of parasite-host interactions involved in pathology and disease
We provide the following resources and expertise
- Protocols and databases related to rodent and human malaria parasites
- Plasmids for genetic modification of rodent and human malaria parasites
- Transgenic and mutant parasite lines (rodent and human malaria parasites)
- Support in generation and characterization of transgenic and mutant parasites
- A database containing information on genetically modified rodent parasite lines: see www.pberghei.eu.
Please contact Dr. Chris J. Janse (https://pberghei.nl/) or Dr. Blandine Franke-Fayard (b.franke-fayard@lumc.nl) for information on protocols, plasmids and transgenic/mutant.
&width=710&height=710)
&width=710&height=710)
Projects
Publications
Team members
- Dr. Chris J Janse (PI)
- Dr. Blandine M.D. Franke-Fayard (PI)
- Dr. Gopal Murugan (PI)
- Ing. Séverine Chevalley (Research technician)
- Ing. Fiona Geurten (Research technician)
- Ing. Jai Ramesar (Research technician)
- Ing. Johannes Kroeze (Research technician)