LUMC sets new standard: neck collar makes most surgeries unnecessary for elderly with neck fractures
Neurosurgeon Jeroen Huybregts.
&width=710&height=710)
By: Lennart 't Hart
Operate or stabilize with a neck collar? For decades, there was debate among doctors treating dens fractures both in the Netherlands and abroad. But until recently, there had never been proof of which option was best. “We are the first to provide that proof,” says Huybregts.
With this, the neurosurgeon set a new standard in the treatment of dens fractures in the elderly. Based on his findings, LUMC now in principle prefers the neck collar over surgery for this patient group.
The results of the study received praise nationally and internationally. The study won four prestigious awards* and the findings were published in the scientific journal Age and Ageing. On Friday, November 21, Huybregts will defend his PhD thesis on the subject.
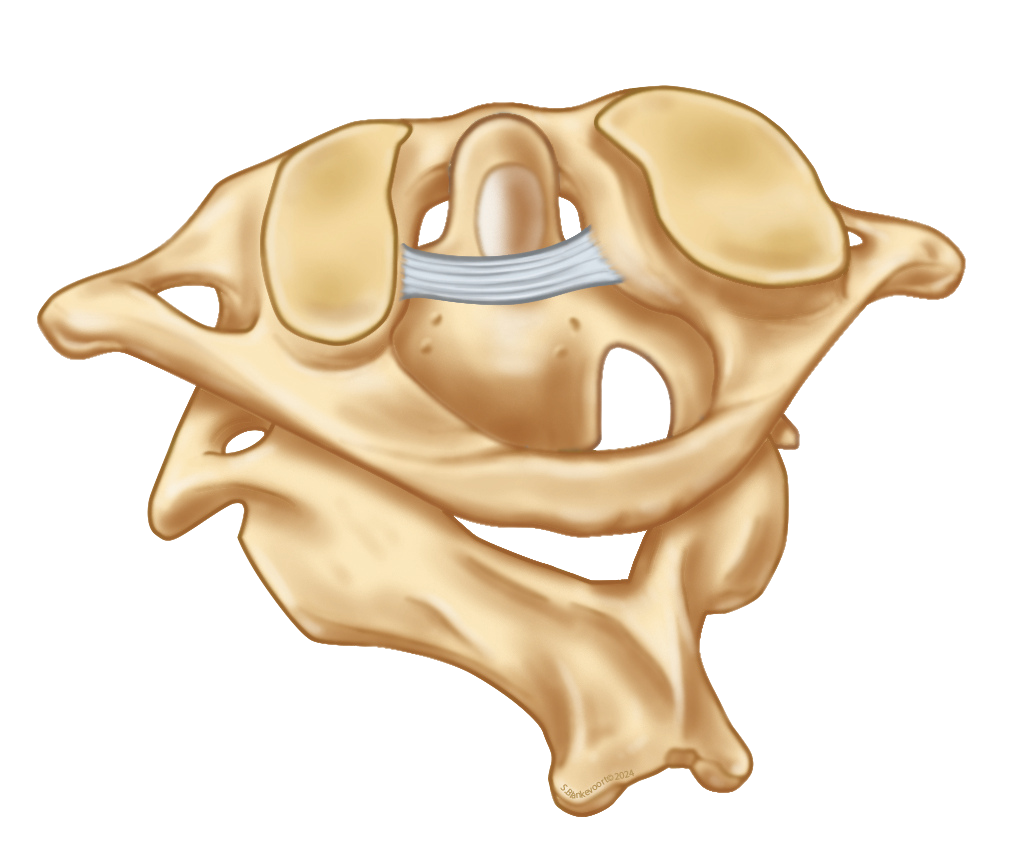
The first two cervical vertebrae, the atlas (top) and the axis (bottom). On the axis sits a bony protrusion: the dens. This part enables head movement but can break in a fall or accident. (Source: S. Blankevoort, 2024)
Axis around which the head rotates
The dens is a bony structure that protrudes upward from the second cervical vertebra. This projection fits into the ring of the first vertebra, allowing the head to rotate. Huybregts: “Your head essentially rotates around the axis of this point. In a dens fracture, this protrusion, the dens, breaks off. In the elderly, this can already happen if they stumble and hit their head against a wall, for example.”
Fear of spinal cord injury unfounded
For a long time, it was assumed that a dens fracture that did not heal properly would cause problems. Huybregts: “In the 1990s, these patients were often confined to bed with a metal frame around their head to prevent movement. The fear was that the fracture would shift backward and press against the spinal cord, causing paralysis. But in practice, that almost never happened. Yet up to a quarter of patients died at the time—not because of the fracture, but due to complications of the treatment, such as pneumonia from lying on their back for too long.”
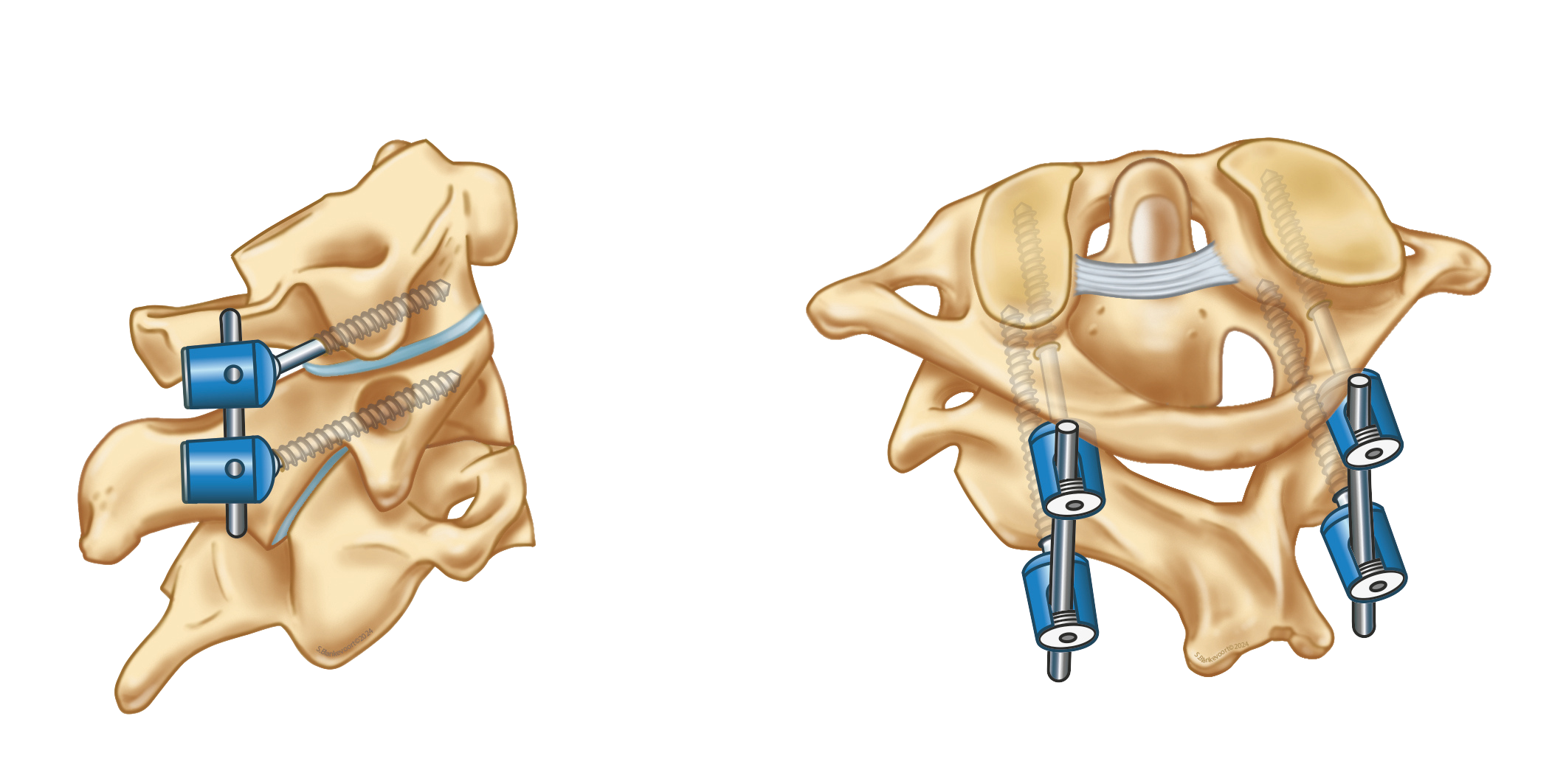
Side and rear view of a surgery in which the first two cervical vertebrae are fused. This procedure provides stability after a dens fracture. (Source: S. Blankevoort, 2024)
Surgery long the standard
Until recently, doctors often chose surgery for a dens fracture. “In this operation, surgeons sometimes fix the dens itself with screws, but more often they fuse the first and second cervical vertebrae. As a result, the vertebrae can no longer rotate relative to each other, making the fracture harmless. Patients are quickly back on their feet, but their head movement is permanently reduced,” says Huybregts.
The idea was that fusing the top two vertebrae would lead to better healing. But this was never properly studied. The same applied to the non-surgical option: usually the neck collar (sometimes a so-called halo vest is used). This hard plastic device stabilizes the cervical vertebrae, allowing the fracture to heal. The collar functions like a cast for a wrist fracture.
Neck collar often sufficient
Huybregts conducted ten years of research into the two treatment options. He concluded that both methods lead to comparable results. In that case, the less invasive treatment—without surgery—is preferable. “Operations are intensive and carry risks, sometimes even fatal. Our study shows that a neck collar is sufficient in most cases,” he says.
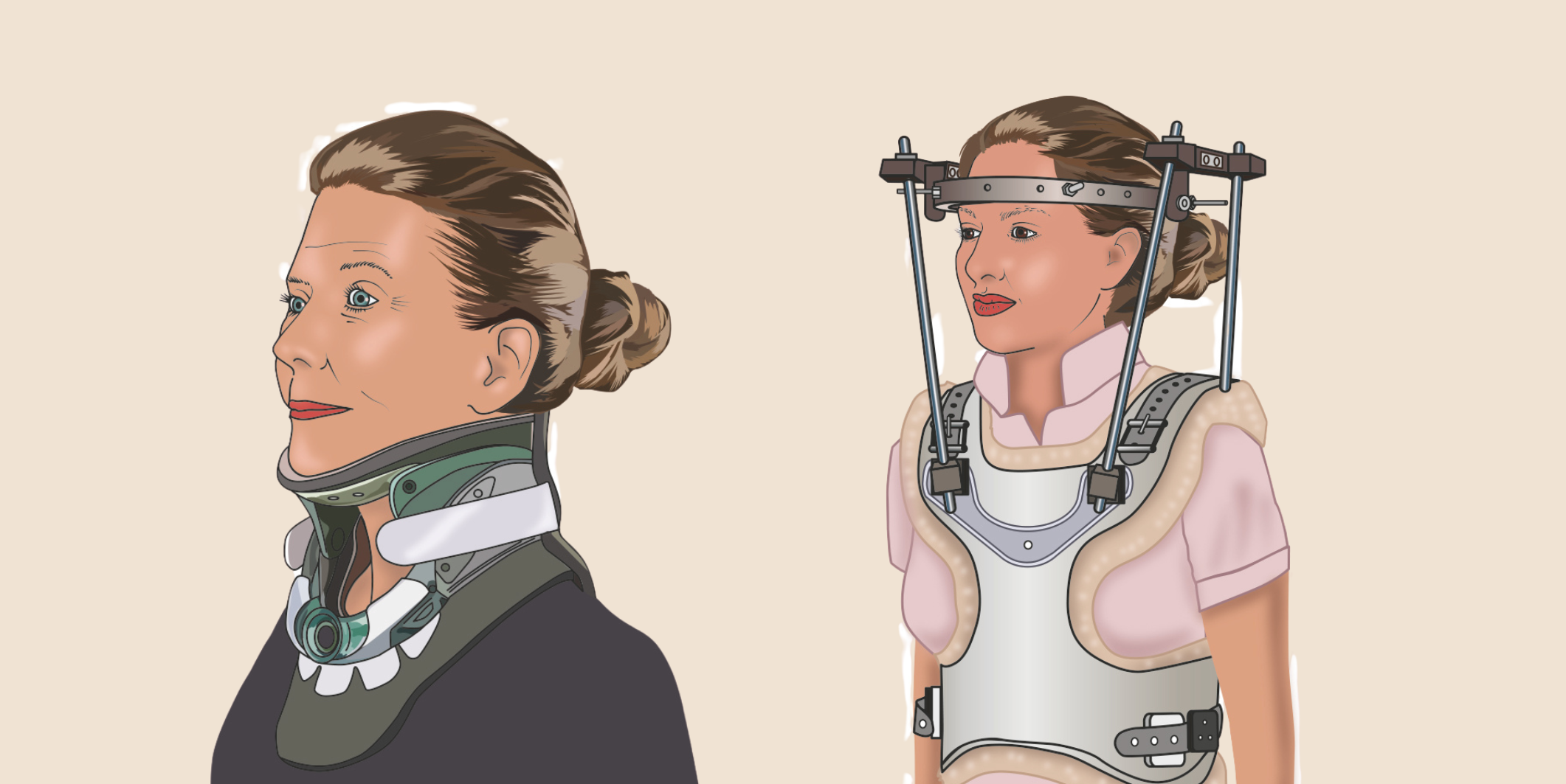
Illustrations of a person with a neck collar (left) and halo vest (right). (Source: S. Blankevoort, 2024)
276 patients from eight countries
Over ten years, the neurosurgeon studied data from 276 patients aged 55 and older from eight European countries. These patients had either undergone surgery or received a neck collar or halo vest (both conservative treatments). He followed them for two years, with five check-ups during that time. This yielded extensive data. “We wanted to know not only how the fracture healed, but also how people functioned in daily life.”
No previous study had examined whether patients actually had complaints or neurological risks after treatment. Our research showed that patients whose fracture did not fully heal had no more complaints than those whose fracture did heal completely. Until now, patients with an incompletely healed fracture were often operated on anyway, even without symptoms. Based on our results, this is unnecessary.”
Choosing the neck collar with confidence
With this study, Huybregts proved that fear of neurological damage after a dens fracture in the elderly is unfounded. Doctors can now choose with greater confidence a less aggressive treatment—preferring a neck collar over surgery.
In some cases, surgery will still be unavoidable, for example if the fracture is very complex or if a patient continues to suffer severe neck pain despite treatment with a collar.
Awards: Best National Spine Society Paper Award (Copenhagen 2025) for best European publication, Dutch Spine Society Award (The Hague 2024) for best Dutch publication, Best Abstract Awards from the European Association of Neurosurgical Societies (Sofia 2024) and Cervical Spine Research Society (Chicago 2024).