Device developed at LUMC helps premature babies breathe again during apnea
&width=710&height=710)
On the NICU (Neonatal Intensive Care Unit) at LUMC, babies who are born extremely prematurely are cared for—some as early as 24 weeks gestation. Because their lungs and brains are not yet fully developed, they may sometimes stop breathing. “The breathing reflex doesn’t always work properly. Also, the chest is much softer, which makes it harder to breathe forcefully,” explains Cramer. “One episode of apnea is not dangerous, but if it happens frequently, it can be harmful. Blood oxygen levels drop quickly during apnea in premature babies, which can ultimately lead to brain damage and developmental delays.”
 Sophie Cramer is a Qualified Medical Engineer and recently obtained her PhD at LUMC. She works four days a week as a staff advisor on the NICU and one day in the Medical Technology department at LUMC.
Sophie Cramer is a Qualified Medical Engineer and recently obtained her PhD at LUMC. She works four days a week as a staff advisor on the NICU and one day in the Medical Technology department at LUMC.
Rubbing the back or tickling the feet
To prevent apnea, doctors and nurses provide positive airway pressure to the lungs via a small mask. This keeps the lungs open and stabilizes them from the inside. Medications, such as caffeine, also help maintain breathing.
Despite these treatments, apneas still occur frequently. When a baby stops breathing in the NICU, an alarm goes off. Nurses then rush to the incubator to try to restart the baby’s breathing. “They do this by rubbing the back or tickling the feet,” says Cramer. “But everyone has their own method. During our study, we counted 57 different techniques.” Over the years, these techniques were often passed from one caregiver to another. None of these methods are scientifically proven, but in practice, they usually work.
Apnea alarms are demanding for staff. “Nurses receive alarms all day and have to rush to the incubator, which doesn’t always happen immediately, according to our research.” Cramer and her team therefore investigated what was already known about automatic stimulation. “We were looking for an extra pair of hands—a device that reacts immediately and stimulates the baby to breathe again while the nurse is on the way,” explains the researcher.
Previous attempts with vibrating mats
Cramer and her team first examined existing research on automatic stimulation for babies with apnea. “We found mattress-like devices that softly vibrate or create waves. But these studies were small, and the devices often remained in the testing phase.” A continuously vibrating mat was also not ideal: “You prefer something that only activates when it’s really needed. That motivated us to continue developing a smart, targeted solution.”
A device that helps
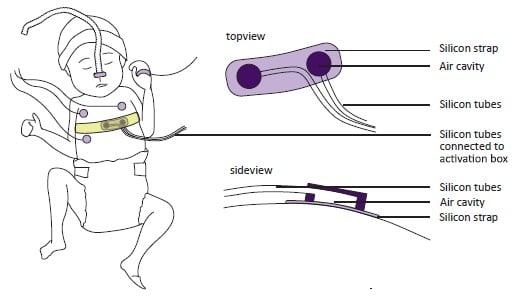 Together with her supervisor Arjan te Pas (Professor of Pediatrics) and the LUMC Design & Prototyping team, Cramer developed BOBBY. “It is a silicone band with two air chambers placed around the baby’s chest. The device is connected to a box with speakers. When the monitor alarm goes off, the speakers start moving. Through airtight silicone tubes, the vibration is transmitted to the air chambers,” she explains. “By activating the chambers in sequence, it feels to the baby like a gentle stroke moving from one side to the other, stimulating the baby to start breathing again.”
Together with her supervisor Arjan te Pas (Professor of Pediatrics) and the LUMC Design & Prototyping team, Cramer developed BOBBY. “It is a silicone band with two air chambers placed around the baby’s chest. The device is connected to a box with speakers. When the monitor alarm goes off, the speakers start moving. Through airtight silicone tubes, the vibration is transmitted to the air chambers,” she explains. “By activating the chambers in sequence, it feels to the baby like a gentle stroke moving from one side to the other, stimulating the baby to start breathing again.”
The idea is simple and clever. The device contains no electronic components, making it safer and more practical. Its design also considers real-world use. “Babies often lie on their parents’ chest for skin-to-skin contact. You can’t take a mat there, but you can use this band.”
Safe and promising
BOBBY is still a prototype—a first version of the product designed to test whether the concept works in practice. The device has been successfully tested at LUMC. “We looked at safety and whether it works as intended,” says Cramer. “The babies remained calm and slept through it. They did not react irritably to the vibration; the comfort score, which nurses record every four hours to measure how comfortable the baby is, remained unchanged while using BOBBY.”
The researcher also noted positive effects of BOBBY on blood oxygen levels. “However, the numbers were still too small to draw definitive conclusions. A larger study would be needed for that.”
Nurses closely involved in the study
During the testing phase, nurses were closely involved. “At first, there was some hesitation. You are automating something they normally do themselves. But positive reactions came quickly. During the study, nurses would tell me if they had a patient who might benefit from the device, which showed that they were thinking along and saw its value.”
Company to further develop device
 Although the device was conceived and tested at LUMC, the hospital is not allowed to market it itself. “LUMC is a healthcare institution, not a manufacturer,” explains Cramer. “Medical device regulations prevent us from producing it for distribution.” Therefore, a spin-off company has been created. This company will further develop the device and obtain CE certification so other hospitals can use it. Cramer and te Pas remain involved as researchers.
Although the device was conceived and tested at LUMC, the hospital is not allowed to market it itself. “LUMC is a healthcare institution, not a manufacturer,” explains Cramer. “Medical device regulations prevent us from producing it for distribution.” Therefore, a spin-off company has been created. This company will further develop the device and obtain CE certification so other hospitals can use it. Cramer and te Pas remain involved as researchers.
If development continues successfully, BOBBY could have a major impact on NICUs. “It automates a manual task that takes a lot of time. If we can do that, nurses can focus on other care tasks, and babies receive help faster.”
Potential to prevent apneas in the future
The next step is to make BOBBY even smarter. “Ideally, we want it not only to react to apnea but also to predict it. For example, it could start vibrating when breathing becomes irregular, potentially preventing apnea altogether,” says Cramer.
In any case, the device shows clear potential. “Less brain damage in premature babies and reduced workload for nurses,” summarizes the researcher. “That would be a huge gain.”
Jonger overleven dankzij technologie
Medische en technologische vooruitgang maakt het mogelijk om baby's steeds jonger en steeds beter in leven te houden. In Nederland ligt de grens om te starten met behandelen op 24 weken. Een kindje dat dan geboren wordt, weegt dan rond de 600 gram.
Hoe jonger de baby, hoe meer ondersteuning die nodig heeft. Baby's die vóór 30 weken zwangerschap ter wereld komen, worden daarom opgenomen op een Neonatale Intensive Care Unit (NICU). Daar krijgen ze intensieve zorg: één verpleegkundige zorgt meestal voor twee baby's, die met geavanceerde technologie voortdurend worden gemonitord en ondersteund.