Artificial Intelligence-based Innovations
Advancing cancer care
The department of Radiation Oncology of the LUMC is involved in multidisciplinary research aimed at improving the treatment and the quality of life of cancer patients, of which image-guided radiation treatment is an important part.
The AI-based Innovations research group aims to innovate the treatment of cancer by 1) developing solutions for tasks that are part of the image-guided radiation treatment workflow which are performed (mostly) manually and involve a time consuming, iterative, and non-insightful process (including the identification of the regions of interest in medical images and the optimization of radiation treatment plans), and 2) enabling better informed and improved clinical decision support to, for example, patient-specifically tailor the follow-up procedure and choice of preferred cancer treatment.
Innovation via an ecosystem of close collaboration
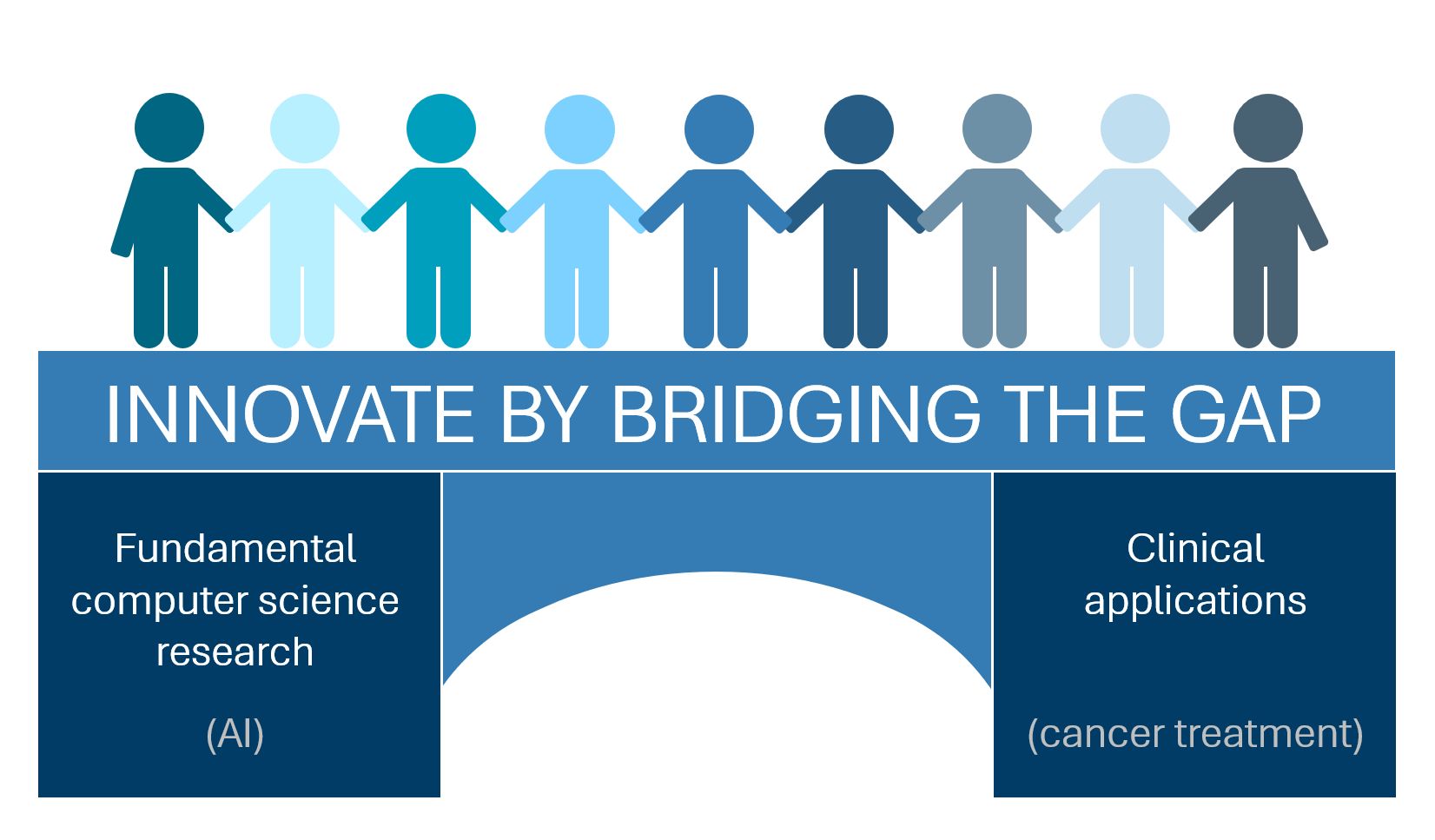
We go beyond the application of AI by closely collaborating with both AI experts who develop new techniques and clinical experts. This results in truly new ways to solve demand-driven challenges coming from the clinic. It also opens the door to understanding what the possibilities and limitations are of the latest techniques and what data we may still need to acquire to realize clinical innovation. In turn, this may raise new questions about how AI techniques should be developed or adapted. In doing so, the cycle of interaction that is central to the ecosystem of innovation, is established.
Three focus areas
Our research can be roughly subdivided into three research focus areas: image processing, optimization of treatment, and explainable AI.
The focus area on image processing includes (semi-)automatic delineation of regions of interest in medical images, and medical image registration (i.e., aligning two medical images). Both are of importance in the process of radiation treatment planning.
The focus area on optimization of treatment currently addresses innovation in internal radiation treatment (i.e., brachytherapy) and, in parallel, will encompass the development of a multi-objective optimization approach for external beam radiation treatment.
Explainable AI can be used for tasks like predictive modelling based on multi-modal data (such as medical images, texts, categories). This way relationships of the underlying data may be revealed. Moreover, the explainability component of these techniques is expected to enlarge the trust in these techniques and thereby the acceptance and clinical uptake.
One of the ultimate goals of the development and application of the explainable AI research projects is to gain improved insights and new knowledge on the relation between cancer treatment as a whole and (late) adverse effects. Not only can image-guided radiation treatment be improved based on this knowledge, also better informed decision making would be enabled regarding the preferred treatment modality (e.g., photon-based radiation treatment versus proton-based radiation treatment) for a specific patient.
Projects
ICAI Lab: Explainable AI for Health (Since 2023)
The Explainable AI for Health Lab is a collaboration between Centrum Wiskunde & Informatica (CWI), Leiden University Medical Center (LUMC), and Amsterdam University Medical Centers – location AMC (Amsterdam UMC).
AI-based clinical decision support has the potential to greatly benefit both physicians and patients. However, many powerful AI models function as “black boxes,” making it difficult to understand how they generate predictions – a barrier to clinical adoption. Researchers at LUMC, Amsterdam UMC, and CWI are developing new forms of AI that lead to models that are inherently explainable as much as possible, enabling clinicians and patients to understand the reasoning behind each prediction.

Themes for Innovation
Our team members
Research team
The following employees of the Department of Radiation Oncology are involved in the scientific research into AI-based innovations:
- Dr. T. Alderliesten, Associate Professor, leader of the Artificial Intelligence-based Innovations research group
- Dr. S.M. de Boer, MD, Radiation Oncologist, LUMC
- Prof.dr. C.L. Creutzberg, MD, Radiation Oncologist, LUMC
- Dr.ir. E.M. Kerkhof, Radiation Oncology Medical Physicist, LUMC
- Prof.dr. Y.M. van der Linden, MD, Radiation Oncologist, Head of Centre of Expertise Palliative Care, LUMC
- Prof.dr. C.R.N. Rasch, MD, Radiation Oncologist, Radiation Oncology Department Chair, LUMC
- L.A. Velema, MD, Radiation Oncologist, LUMC
- L.A.L. Verhagen, Radiation Therapy Technologist, LUMC
Research team
The following employees of the Department of Radiation Oncology are involved in the scientific research into AI-based innovations:
- Dr. T. Alderliesten, Associate Professor, leader of the Artificial Intelligence-based Innovations research group
- Dr. S.M. de Boer, MD, Radiation Oncologist, LUMC
- Prof.dr. C.L. Creutzberg, MD, Radiation Oncologist, LUMC
- Dr.ir. E.M. Kerkhof, Radiation Oncology Medical Physicist, LUMC
- Prof.dr. Y.M. van der Linden, MD, Radiation Oncologist, Head of Centre of Expertise Palliative Care, LUMC
- Prof.dr. C.R.N. Rasch, MD, Radiation Oncologist, Radiation Oncology Department Chair, LUMC
- L.A. Velema, MD, Radiation Oncologist, LUMC
- L.A.L. Verhagen, Radiation Therapy Technologist, LUMC
Current members
- G. Andreadis, PhD student, LUMC
- A. Chebykin, PhD student, CWI / TU Delft
- L.R.M. Dickhoff, PhD student, LUMC
- A. Guijt, PhD student, CWI / TU Delft
- D.M.F. Ha, PhD student, LUMC
- J. Harrison, PhD student, CWI / TU Delft
- J. Koch, PhD student, CWI / TU Delft
- E. Kostoulas, PhD student, LUMC
- M. Malafaia, PhD student, CWI / TU Delft
- P. Mendes Antunes De Matos (Scientific Programmer, CWI)
- C.J. Rodriguez, PhD student, LUMC
- C.J.A. Romme, PhD student, Amsterdam UMC / UvA
- T. Schlender, PhD student, LUMC
- R.J. Scholman, PhD student, CWI / TU Delft
- E.M.C. Sijben, PhD student, CWI / LUMC
Former members
- Dr. T.M. Deist
- H.H. Deuzeman
- Dr. A. Dushatskiy
- Dr. M. Grewal
- E.C. Harderwijk
- J.J. Roorda, MD
- T. Uriot
- W. Visser-Groot
- J. de Vries
Collaborations
Within the LUMC, the research group works together with, among others, the department of Otorhinolaryngology (Prof.dr. J.C. Jansen), the department of Radiology (Dr. B.M. Verbist), and the Division of Image Processing (Laboratorium voor Klinische en Experimentele Beeldverwerking, LKEB) (Prof.dr.ir. M. Staring). Further, the research group has links with the Clinical AI Implementation and Research Lab (CAIRELab) of the LUMC.
Outside of the LUMC, there is close collaboration in the Netherlands with the national research institute for mathematics and computer science in the Netherlands (Centrum Wiskunde & Informatica, CWI) (Prof.dr. P.A.N. Bosman (part-time professor at TU Delft) and Dr.ir. P.A. Bouter (scientific software developer)). We further collaborate with Utrecht University (Dr.ir. D. Thierens), the departments of Radiation Oncology and Gynaecology of the Amsterdam UMC (Drs. D.L.J. Barten, H.H. Deuzeman, Dr. K. A. Hinnen, Dr. L.R.C.W. van Lonkhuijzen, Dr. B.R. Pieters, Prof.dr. L.J.A. Stalpers, Dr. J. Wiersma), the department of Radiation Oncology of the Erasmus MC Cancer Institute (Dr. G.H. Westerveld), and the departments of Radiation Oncology of Catharina Hospital Eindhoven, UMC Groningen, Maastro clinic, The Netherlands Cancer Institute, Radboud UMC, and UMC Utrecht. Moreover, there is close collaboration with the departments of Pathology and Radiology of The Netherlands Cancer Institute, and the larger DIRECT-DCIS consortium.
…Within the LUMC, the research group works together with, among others, the department of Otorhinolaryngology (Prof.dr. J.C. Jansen), the department of Radiology (Dr. B.M. Verbist), and the Division of Image Processing (Laboratorium voor Klinische en Experimentele Beeldverwerking, LKEB) (Prof.dr.ir. M. Staring). Further, the research group has links with the Clinical AI Implementation and Research Lab (CAIRELab) of the LUMC.
Outside of the LUMC, there is close collaboration in the Netherlands with the national research institute for mathematics and computer science in the Netherlands (Centrum Wiskunde & Informatica, CWI) (Prof.dr. P.A.N. Bosman (part-time professor at TU Delft) and Dr.ir. P.A. Bouter (scientific software developer)). We further collaborate with Utrecht University (Dr.ir. D. Thierens), the departments of Radiation Oncology and Gynaecology of the Amsterdam UMC (Drs. D.L.J. Barten, H.H. Deuzeman, Dr. K. A. Hinnen, Dr. L.R.C.W. van Lonkhuijzen, Dr. B.R. Pieters, Prof.dr. L.J.A. Stalpers, Dr. J. Wiersma), the department of Radiation Oncology of the Erasmus MC Cancer Institute (Dr. G.H. Westerveld), and the departments of Radiation Oncology of Catharina Hospital Eindhoven, UMC Groningen, Maastro clinic, The Netherlands Cancer Institute, Radboud UMC, and UMC Utrecht. Moreover, there is close collaboration with the departments of Pathology and Radiology of The Netherlands Cancer Institute, and the larger DIRECT-DCIS consortium.
International collaboration is taking place with the Aarhus University Hospital in Denmark (Dr. S. Buus, Dr. J. Graversen Johansen, A. Traberg Hansen), the Virginia Commonwealth University in the USA (Prof.dr. D.A. Todor, E. Garlock), the Medical University of Vienna in Austria (Dr. C. Kirisits, Dr. N. Eder-Nesvacil), and the Victoria University of Wellington in New Zealand (Prof. M. Zhang, Dr. A. Lensen), Wellington Regional Hospital in New Zealand (Dr. L. Aldrovandi, S. Bulling, S. Hewitt). Moreover, there is collaboration with the Association for Research and Development of the Faculty of Medicine – CCUL (AIDFM), and the larger FH-EARLY consortium.