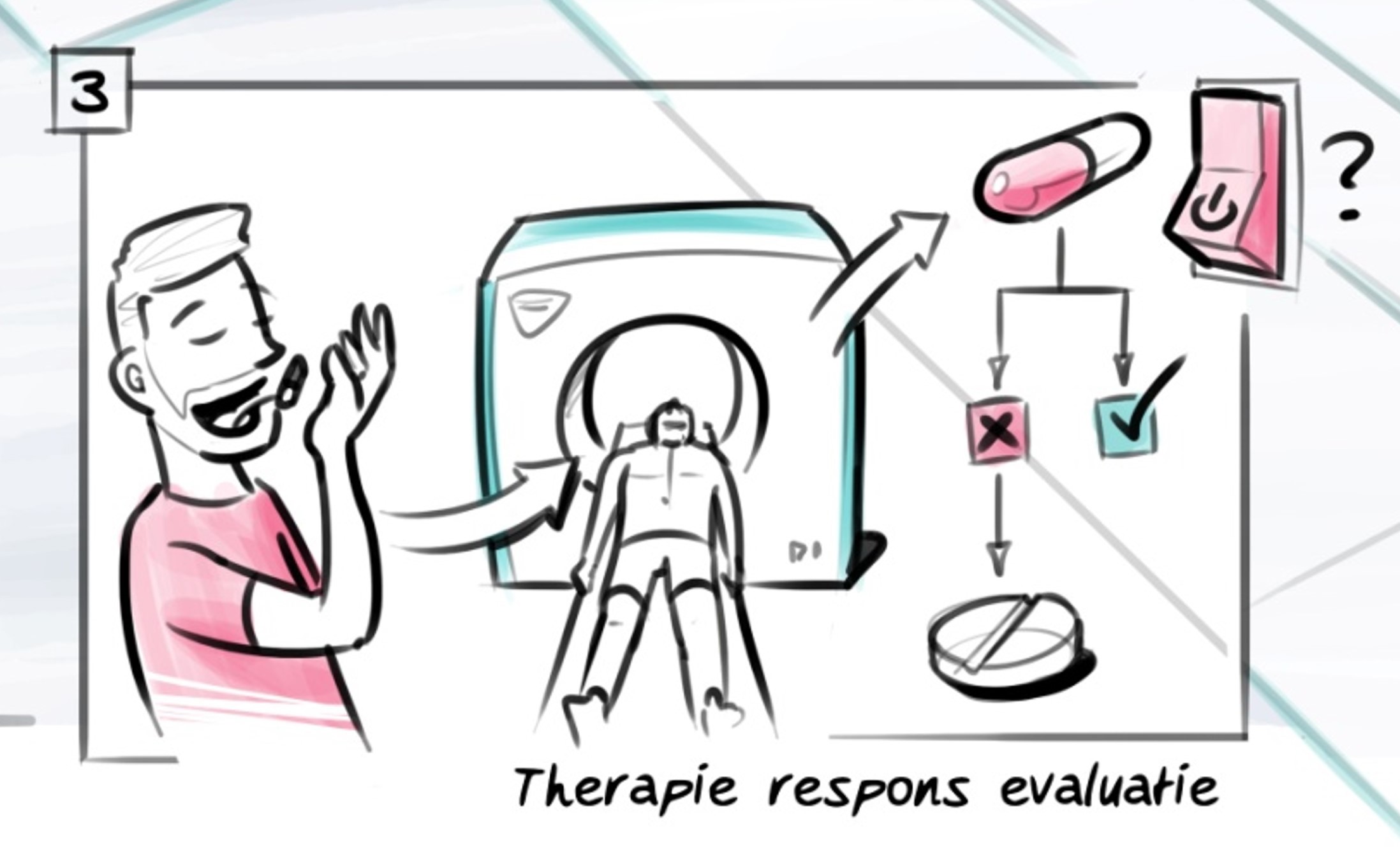
Nuclear Medicine
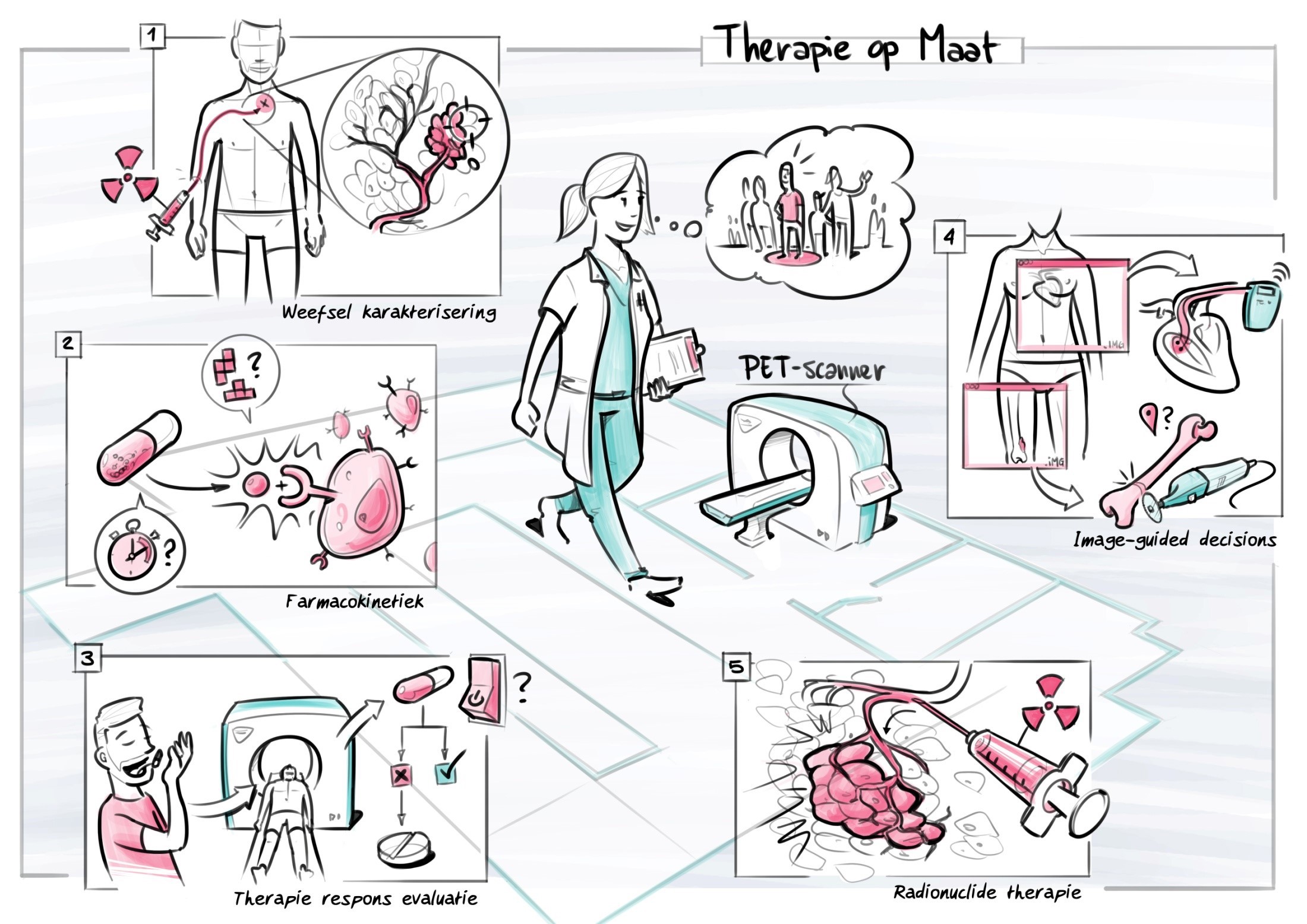
Tissue Characterization
Molecular imaging is a technique that allows the non-invasive imaging of molecular targets. As an imaging technique, Positron Emission Tomography (PET) has two unique characteristics: a very high sensitivity (at the picomolar level) and the possibility of visualisation and quantification of molecular processes and targets under investigation. Primarily, however, PET offers the opportunity to obtain pathophysiological information from living patients in a non-invasive and quantified way. Examples here would include the imaging of metabolism, perfusion, hypoxia, proliferation, amino-acid transport, angiogenesis, necrosis, apoptosis, inflammation, receptor status, receptor occupancy, drug delivery, cell-tracking, stem cell delivery / viability / differentiation, sympathetic innervation, enzyme activity, metabolite concentration, peptide concentration etc.
…Tissue Characterization
Molecular imaging is a technique that allows the non-invasive imaging of molecular targets. As an imaging technique, Positron Emission Tomography (PET) has two unique characteristics: a very high sensitivity (at the picomolar level) and the possibility of visualisation and quantification of molecular processes and targets under investigation. Primarily, however, PET offers the opportunity to obtain pathophysiological information from living patients in a non-invasive and quantified way. Examples here would include the imaging of metabolism, perfusion, hypoxia, proliferation, amino-acid transport, angiogenesis, necrosis, apoptosis, inflammation, receptor status, receptor occupancy, drug delivery, cell-tracking, stem cell delivery / viability / differentiation, sympathetic innervation, enzyme activity, metabolite concentration, peptide concentration etc.
Currently we have studies running to determine the tumour expression of PD-1, ER, that determine the nature of cytologically indeterminate thyroid nodules, to determine the role of radiomics analyses in various neoplasms, to determine the clinical benefit of folate receptor imaging prior to surgery, to image tumor angiogenesis using [18F]-Fluciclatide PET/CT in patients with colorectal and pancreatic cancer, to image expression of prostate specific membrane antigen (PSMA) using [18F]-DCFPyL PET/CT in patients with colon and gastric cancer and [18F]-JK-PSMA-7 in patients with advanced sarcoma and urothelial cell carcinomas, to clinically translate Integrin αvβ6-targeted multimodality molecular imaging for pancreatic cancer detection, to evaluate diagnostic performance of [89Zr]-girentuximab to non-invasively detect clear cell renal cell carcinoma in patients with indeterminate renal masses and molecular imaging techniques are used to investigate human brown adipose tissue thermogenesis.
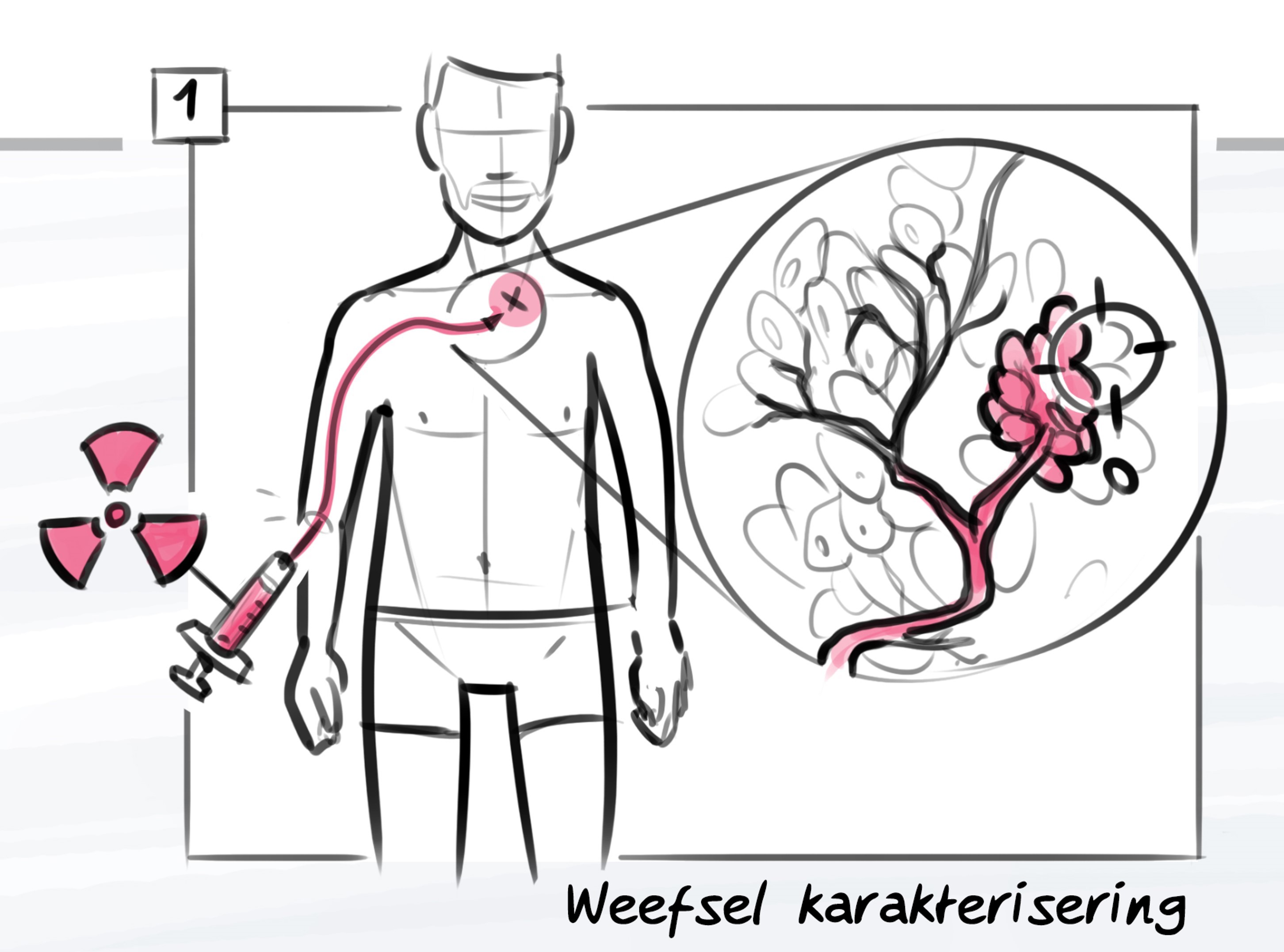
Pharmacokinetics of Therapies
As it allows the in vivo and non-invasive local measurement of receptor occupancy and the inhibition of enzymes in tissue, PET is offering unique opportunities for evaluating new drugs. It enables one to determine with a high degree of accuracy whether a particular medicine is indeed operating on the desired target. Its specific properties also make it an appropriate technique for personalized medicine, that is, for delivering the right medicine in the right dose to the right patient. This could improve quality of life while simultaneously reducing cost by not unnecessarily treating patients with expensive medicines that do not benefit them. All this will help to achieve better care at lower cost, although a lot of research needs to be done before such methods will be accepted by health insurance companies and be included in Diagnosis-Treatment Combinations (DBCs).
…Pharmacokinetics of Therapies
As it allows the in vivo and non-invasive local measurement of receptor occupancy and the inhibition of enzymes in tissue, PET is offering unique opportunities for evaluating new drugs. It enables one to determine with a high degree of accuracy whether a particular medicine is indeed operating on the desired target. Its specific properties also make it an appropriate technique for personalized medicine, that is, for delivering the right medicine in the right dose to the right patient. This could improve quality of life while simultaneously reducing cost by not unnecessarily treating patients with expensive medicines that do not benefit them. All this will help to achieve better care at lower cost, although a lot of research needs to be done before such methods will be accepted by health insurance companies and be included in Diagnosis-Treatment Combinations (DBCs).
Currently, a study is running to investigate whether [89Zr]-bevacizumab PET/CT imaging of vestibular schwannomas can upfront predict bevacizumab treatment efficacy in patients with symptomatic neurofibromatosis type 2.
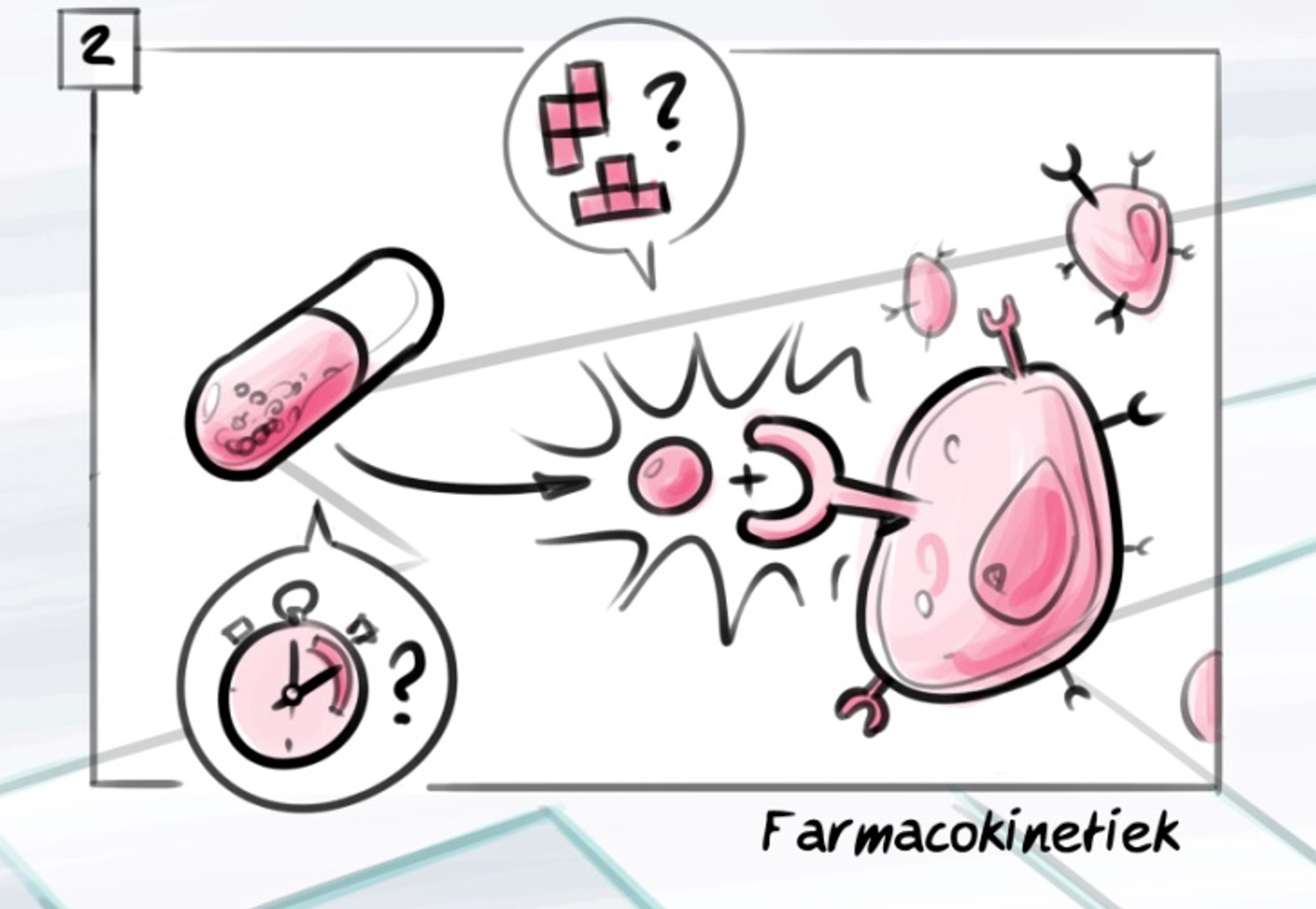
Therapy Response Evaluation
Molecular imaging can show at an early stage of therapy whether a therapy is effective. This will enable early response evaluation of many kinds of treatments, such as antibiotics, anti-arthritis medication, anti-ischaemic therapy, chemotherapy, targeted therapy, radiotherapy, proton therapy, etc. Duration of treatment, dose intensity, and treatment change decisions will be much better adjusted to the biological behaviour of a disease in an individual patient.
Currently studies are running on hypoxia imaging in proton therapy, on PSMA-expression in advanced sarcoma and urothelial cell carcinomas, to study the activation of human brown adipose tissue by medication, to identify predictive PET/CT imaging biomarkers (radiomics) for the efficacy of afatinib treatment, to assess whether radiomics extracted from pretreatment PET/CT in locally advanced cervical cancer patients, treated with neoadjuvant chemoradiotherapy followed by surgery, could be used to identify responders, to investigate the performance of [18F]-NaF PET/CT to monitor treatment response of fibrous dysplasia to RANK1-inhibition and to investigate the performance of [89Zr]trastuzumab PET/CT imaging of HER2 positive breast cancer for predicting pathologic complete response after neoadjuvant chemotherapy.
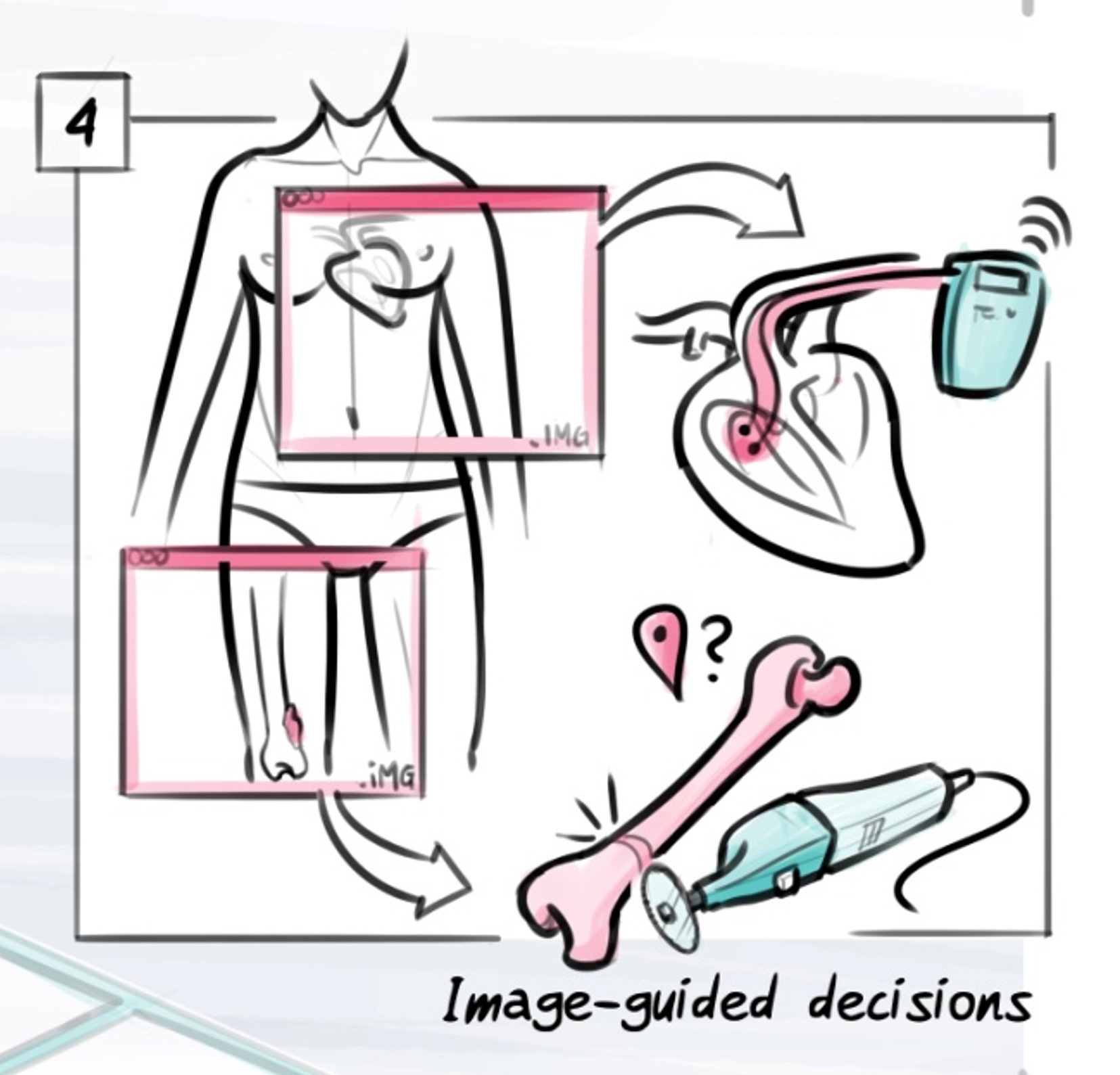
Image-Guided Decisions
These may include:
- the targeted extraction of biopsies guided by molecular imaging, which will help to prevent sampling error;
- operation site marking by molecular imaging, which will guarantee free margins of resection during the operation. Molecular imaging, moreover, can also be helpful in conducting organ-conserving therapies. Preserving organ function means shorter hospitalization periods, shorter rehabilitation time, and better quality of life;
…Image-Guided Decisions
These may include:
- the targeted extraction of biopsies guided by molecular imaging, which will help to prevent sampling error;
- operation site marking by molecular imaging, which will guarantee free margins of resection during the operation. Molecular imaging, moreover, can also be helpful in conducting organ-conserving therapies. Preserving organ function means shorter hospitalization periods, shorter rehabilitation time, and better quality of life;
- molecular imaging may help to make radiotherapy planning more accurate, making sure that radioresistant parts of the tumour receive a higher dose while reducing toxicity on healthy tissue as much as possible. All this should bring about improved local control, decreased toxicity, and prolonged survival. Imaging can help to decide when and where to intensify the treatment and when to opt for conservative strategies if aggressive intervention is unnecessary. This will help to reduce negative effects in the long term.
Currently, we are investigating new imaging criteria for non-operative treatment following neoadjuvant chemoradiation in rectal cancer patients, we are investigating the added value of digital PET in (re)staging patients with pancreatic cancer, we perform in-vivo dosimetry for eye, brain and head and neck proton radiation, we assess de-escalating diagnostics and treatment in the management of papillary thyroid cancer, we evaluate [18F]-FDG-PET/CT in children with suspected infection or inflammation, we investigate the added value of multimodality imaging for personalizing sarcoma care and in the care of patients with gastrointestinal stromal tumours (GIST) and we evaluate the impact on management decision making of molecular breast imaging.
Radionuclide Therapy
Several tracers that can be used for diagnostics can also be labelled with a radionuclide for therapy, such as alpha- and beta-radiation. Prior to therapy, dosimetry can also be performed with the diagnostic radionuclide to obtain a reliable assessment of the balanced administrable activity optimised for maximum therapeutic effects but minimal toxicity to critical organs at risk (pre-treatment dosimetry, quantitative PET or SPECT). Immediately after therapy, imaging can help to measure the dose that has actually been delivered to the treated tissue (post-treatment dosimetry, mostly SPECT). These are new and promising therapies in the treatment of metastasized prostate carcinomas ([177Lu]-PSMA), neuroendocrinological tumours ([177Lu]-DOTATATE), hepatocellular carcinomas (SIRT), liver metastases (SIRT), painful bone metastases (radium-223), malignant lymphomas, thyroid diseases (131I), arthritic diseases, etc.
…Radionuclide Therapy
Several tracers that can be used for diagnostics can also be labelled with a radionuclide for therapy, such as alpha- and beta-radiation. Prior to therapy, dosimetry can also be performed with the diagnostic radionuclide to obtain a reliable assessment of the balanced administrable activity optimised for maximum therapeutic effects but minimal toxicity to critical organs at risk (pre-treatment dosimetry, quantitative PET or SPECT). Immediately after therapy, imaging can help to measure the dose that has actually been delivered to the treated tissue (post-treatment dosimetry, mostly SPECT). These are new and promising therapies in the treatment of metastasized prostate carcinomas ([177Lu]-PSMA), neuroendocrinological tumours ([177Lu]-DOTATATE), hepatocellular carcinomas (SIRT), liver metastases (SIRT), painful bone metastases (radium-223), malignant lymphomas, thyroid diseases (131I), arthritic diseases, etc.
Currently we have studies running in redifferentiation of radioiodine refractory thyroid cancer, we are evaluating if [166Ho]-microsphere treatments can be quantified accurately in multicenter SPECT/CT studies, we perform a dose finding study on [166Ho]-radioembolization as adjuvant treatment to radiofrequency ablation for early stage hepatocellular carcinoma, we analyse [90Y]-radioembolization in hepatocellular carcinoma patients and we are currently preparing for the next big innovation wave in our field: radionuclide therapy with [177Lu]-PSMA. Hopefully, we will soon become one of the Theranostic Centers in the Netherlands.
Group Leaders
Prof. dr. Lioe-Fee de Geus-Oei, MD PhD
- Nuclear Medicine Physician
- Lioe-Fee de Geus-Oei - Leiden University (universiteitleiden.nl)
- Lioe-Fee de Geus-Oei (0000-0003-1817-2743) (orcid.org)
Dr. Dennis Vriens, MD PhD
- Nuclear Medicine Physician
- Dennis Vriens (linkedin.com)
- Dennis Vriens (0000-0001-5762-6766) (orcid.org)
Group Leaders
Prof. dr. Lioe-Fee de Geus-Oei, MD PhD
- Nuclear Medicine Physician
- Lioe-Fee de Geus-Oei - Leiden University (universiteitleiden.nl)
- Lioe-Fee de Geus-Oei (0000-0003-1817-2743) (orcid.org)
Dr. Dennis Vriens, MD PhD
- Nuclear Medicine Physician
- Dennis Vriens (linkedin.com)
- Dennis Vriens (0000-0001-5762-6766) (orcid.org)
Dr. Linda Heijmen, MD PhD
- Nuclear Medicine Physician
- (99+) Linda Heijmen | LinkedIn
- Linda Heijmen (0000-0003-1453-3337) (orcid.org)
Dr. Floris van Velden, PhD
- Medical Physicist Expert
- Floris van Velden (linkedin.com)
- Floris van Velden (0000-0003-2859-2119) (orcid.org)
Group Members
Dr. ir. Mette Stam, PhD
- Medical Physicist Expert
Dr. Tom Molenaar, PhD
- Radiochemist
- https://www.linkedin.com/in/tom-molenaar-ba02b9117/
- https://orcid.org/my-orcid?orcid=0000-0002-6110-1142
Dr. Martin Pool, PhD
- Radiopharmacist
- https://www.linkedin.com/in/martin-pool-91119120/
- https://orcid.org/my-orcid?orcid=0000-0002-4892-3109
Drs. Daphne Rietbergen, MD
- Nuclear Medicine Physician
- ORCID nr 0000 0001 9873 6179
Dr. Lenka Pereira Arias-Bouda, MD PhD
- Nuclear Medicine Physician
- https://orcid.org/my-orcid?orcid=0000-0002-6879-5554
Drs. Frits Smit, MD
- Nuclear Medicine Physician
Drs. Richard Raghoo, MD
- Nuclear Medicine Physician
- https://nl.linkedin.com/in/richard-raghoo-055a3066
Petra Dibbets-Schneider
- Research Technologist
Drs. Eidrees Ghariq, MD
- Nuclear Medicine Physician
Drs. Isabeau Ciggaar, MD
- Resident in Nuclear Radiology
- LinkedIn: https://nl.linkedin.com/in/isabeau-ciggaar-419a3498
- ORCID: https://orcid.org/0000-0003-1375-5157
Alina van de Burgt, MSc
- Technical Physician
- https://www.linkedin.com/in/alinavandeburgt/
- ORCID: 0000-0001-8170-0583
PhD Candidates
Drs. Wouter van der Bruggen, MD
- Nuclear Medicine Physician
- ORCID identifier: 0000-0002-4689-6506 (orcid.org)
- https://www.linkedin.com/in/woutervanderbruggen/
Drs. Christinne Corion, MD
- Resident in Surgery
- https://www.linkedin.com/in/christinne-corion-61968614a
Maaike Dotinga, MSc
- Technical Physician
- Maaike Dotinga (linkedin.com)
- Maaike Dotinga (0000-0002-8384-7164) (orcid.org)
Pim Hendriks, MSc
- Technical Physician
- Pim Hendriks (LinkedIn)
- Pim Hendriks (0000-0002-4992-9967) (orcid.org)
Timo Kalisvaart, MD
- ORCID identifier: 0000-0003-3531-3640 (orcid.org)
Fleur Kleiburg, MD
Lisanne de Koster, MD
- Resident in Surgery
- https://www.linkedin.com/in/lisanne-de-koster-b0423678/
- ORCID: 0000-0001-8111-1172
Wyanne Noortman, MSc
- Technical Physician
- Wyanne Noortman (linkedin.com)
- Wyanne Noortman (0000-0003-0450-951X) (orcid.org)
Sofia Carrilho Vaz, MD
- Nuclear Medicine Physician
- https://www.linkedin.com/in/sofia-c-vaz-26b11b189/
- ORCID identifier: 0000-0003-4229-9349
&width=2200)
&width=2904)
&width=2074)
&width=2195)
&width=1655)
&width=2114)