Ocular MRI
Conventional ophthalmic imaging techniques, such as fundus photography, have intrinsic limitations as they do not provide 3D visualisation of the eye and cannot image inside opaque tissues, such as a tumour. MRI could resolve many of these limitations, but conventional MR-images of the eye are of low diagnostic value due eye motion induced artefacts and the high spatial resolution needed to differentiate the ocular structures. We develop eye-specific MRI techniques, such as a dedicated eye-coil and acquisition strategies, to resolve these challenges and enable high resolution ocular MR-imaging in a clinical setting. Together with our collaborators, especially from ophthalmology and radiotherapy, we apply and evaluate these new possibilities of MRI for various ocular conditions.
…Conventional ophthalmic imaging techniques, such as fundus photography, have intrinsic limitations as they do not provide 3D visualisation of the eye and cannot image inside opaque tissues, such as a tumour. MRI could resolve many of these limitations, but conventional MR-images of the eye are of low diagnostic value due eye motion induced artefacts and the high spatial resolution needed to differentiate the ocular structures. We develop eye-specific MRI techniques, such as a dedicated eye-coil and acquisition strategies, to resolve these challenges and enable high resolution ocular MR-imaging in a clinical setting. Together with our collaborators, especially from ophthalmology and radiotherapy, we apply and evaluate these new possibilities of MRI for various ocular conditions.
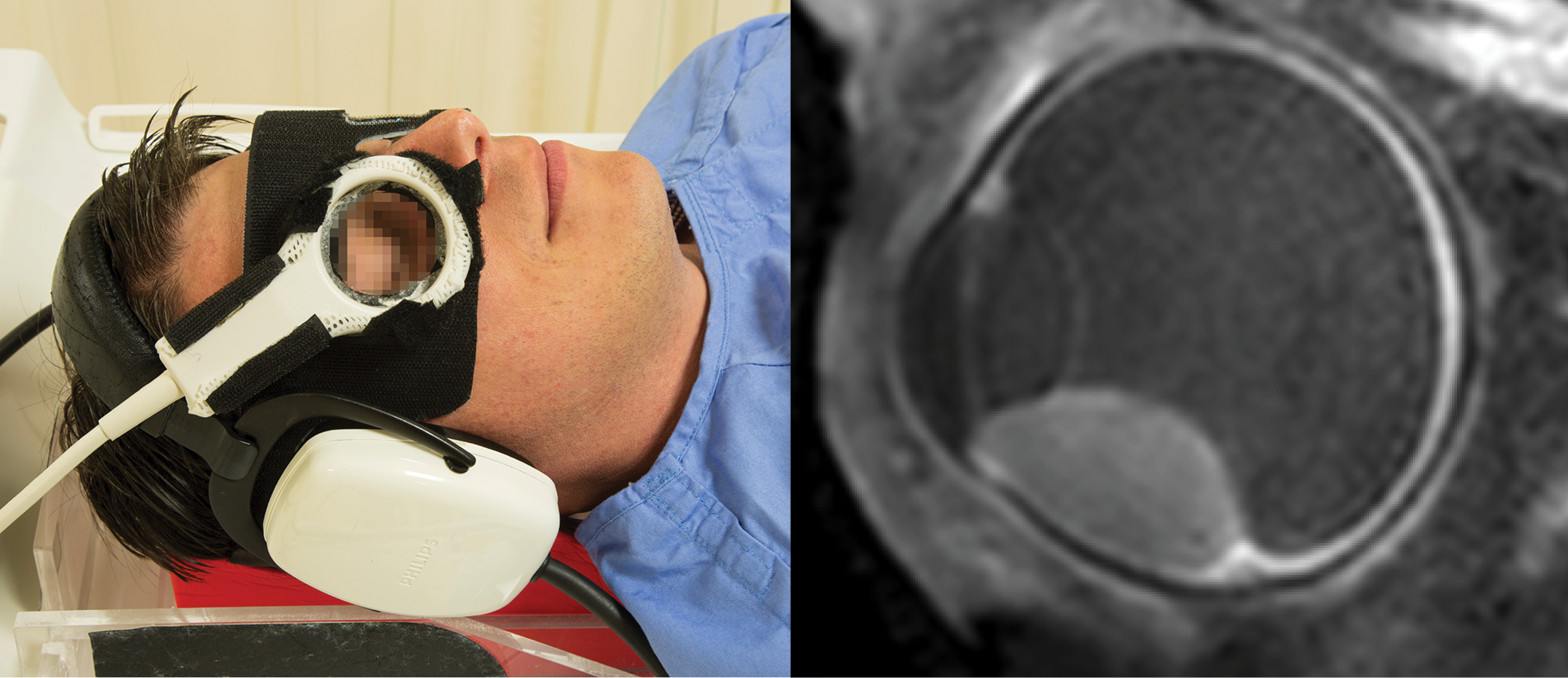
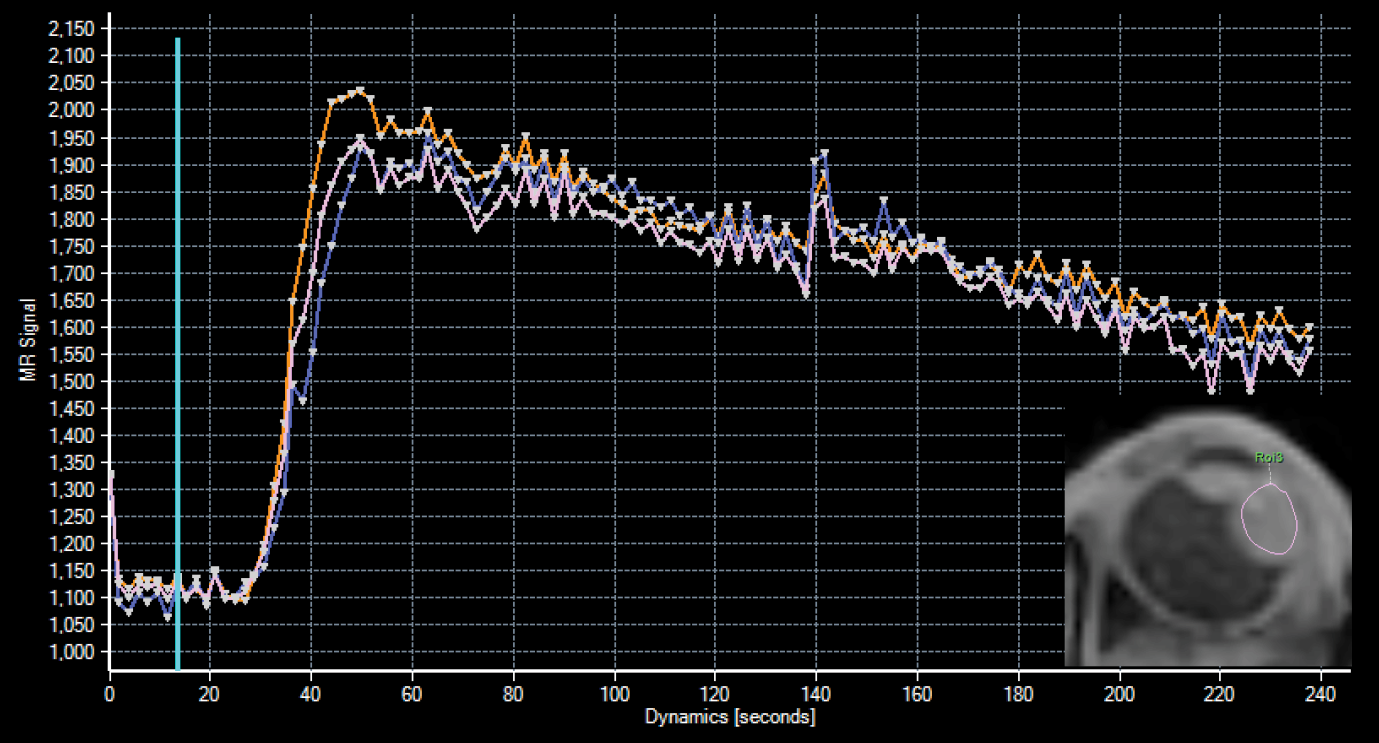
As the LUMC is the national reference center for Uveal Melanoma, the most common primary intra-ocular tumour, a large part of our research focusses on using MRI to improve the care for these patients. We develop eye-specific quantitative MRI techniques, such as perfusion weighted imaging, to aid in the diagnosis of uveal melanoma and to evaluate if they can be used as an early marker of therapy response. Together with the Holland Proton Therapy Center, we are developing MR-based ocular proton therapy planning to reduce its side-effects, such as vision loss.
…As the LUMC is the national reference center for Uveal Melanoma, the most common primary intra-ocular tumour, a large part of our research focusses on using MRI to improve the care for these patients. We develop eye-specific quantitative MRI techniques, such as perfusion weighted imaging, to aid in the diagnosis of uveal melanoma and to evaluate if they can be used as an early marker of therapy response. Together with the Holland Proton Therapy Center, we are developing MR-based ocular proton therapy planning to reduce its side-effects, such as vision loss.
Projects
Themes for Innovation
Key publications
Team members
Current members:
- Jan-Willem Beenakker, PI
- Corné Haasjes, PhD candidate
- Lennart Pors, PhD candidate
- Lisa Klaassen, PhD candidate
- Martijn Hol, PhD candidate
- Michael Tang, PhD candidate
- Bas van der Burgh, PhD candidate

Former members:
- Kevin Keene, PhD candidate
- Luc van Vught, PhD candidate
- Lorna Grech-Fonk, PhD candidate
- Myriam Jaarsma-Coes, PhD candidate
- Teresa Ferreira, PhD candidate